Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Synchrotron microbeam irradiation induces neutrophil infiltration, thrombocyte attachment and selective vascular damage in vivo.
Scientific Reports ( IF 3.8 ) Pub Date : 2016-09-19 , DOI: 10.1038/srep33601 Daniel Brönnimann , Audrey Bouchet , Christoph Schneider , Marine Potez , Raphaël Serduc , Elke Bräuer-Krisch , Werner Graber , Stephan von Gunten , Jean Albert Laissue , Valentin Djonov
Scientific Reports ( IF 3.8 ) Pub Date : 2016-09-19 , DOI: 10.1038/srep33601 Daniel Brönnimann , Audrey Bouchet , Christoph Schneider , Marine Potez , Raphaël Serduc , Elke Bräuer-Krisch , Werner Graber , Stephan von Gunten , Jean Albert Laissue , Valentin Djonov
|
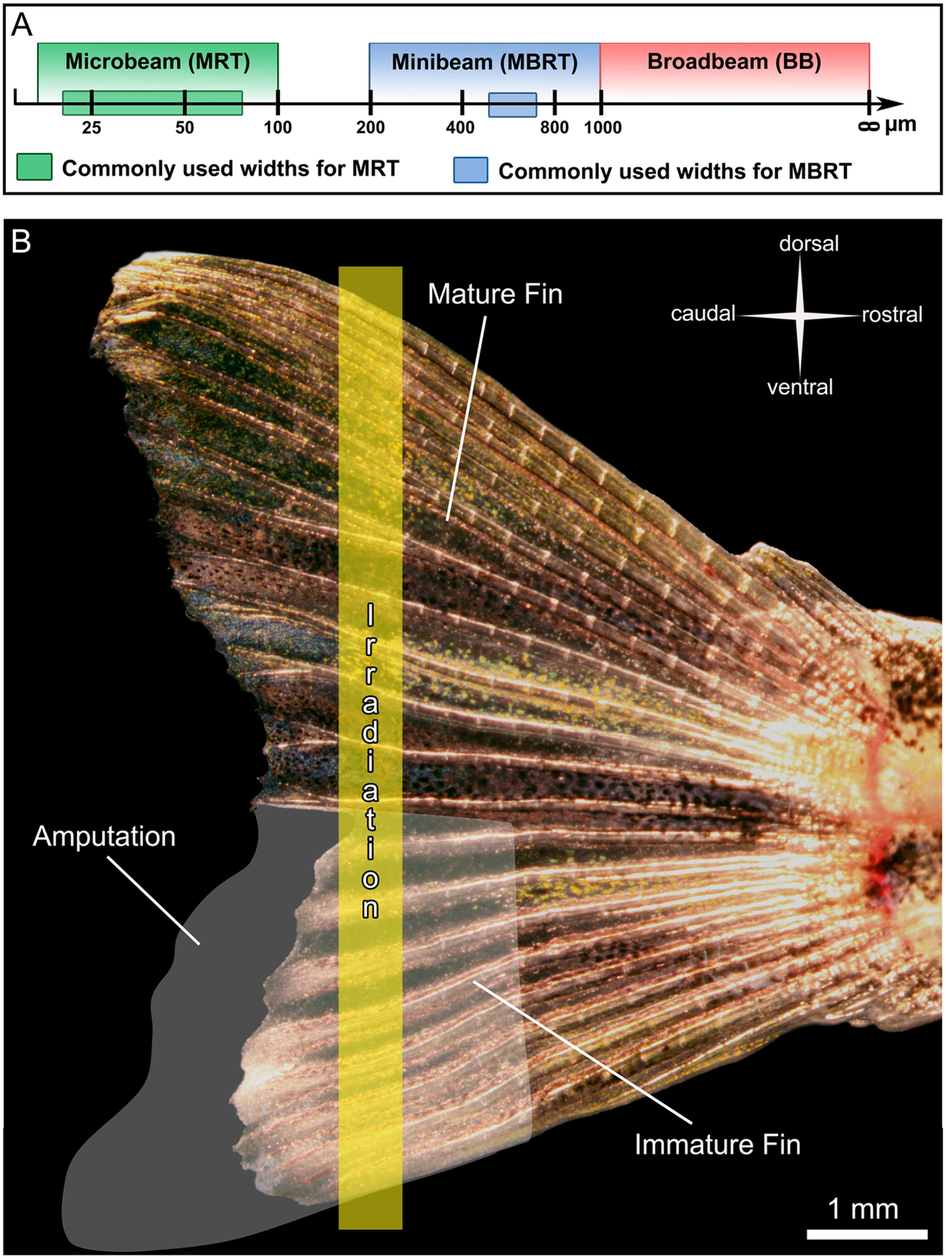
Our goal was the visualizing the vascular damage and acute inflammatory response to micro- and minibeam irradiation in vivo. Microbeam (MRT) and minibeam radiation therapies (MBRT) are tumor treatment approaches of potential clinical relevance, both consisting of parallel X-ray beams and allowing the delivery of thousands of Grays within tumors. We compared the effects of microbeams (25-100 μm wide) and minibeams (200-800 μm wide) on vasculature, inflammation and surrounding tissue changes during zebrafish caudal fin regeneration in vivo. Microbeam irradiation triggered an acute inflammatory response restricted to the regenerating tissue. Six hours post irradiation (6 hpi), it was infiltrated by neutrophils and fli1a(+) thrombocytes adhered to the cell wall locally in the beam path. The mature tissue was not affected by microbeam irradiation. In contrast, minibeam irradiation efficiently damaged the immature tissue at 6 hpi and damaged both the mature and immature tissue at 48 hpi. We demonstrate that vascular damage, inflammatory processes and cellular toxicity depend on the beam width and the stage of tissue maturation. Minibeam irradiation did not differentiate between mature and immature tissue. In contrast, all irradiation-induced effects of the microbeams were restricted to the rapidly growing immature tissue, indicating that microbeam irradiation could be a promising tumor treatment tool.
中文翻译:

同步辐射在体内诱导中性粒细胞浸润,血小板附着和选择性血管损伤。
我们的目标是可视化体内对微束和微束照射的血管损伤和急性炎症反应。微型束(MRT)和微型束放射疗法(MBRT)是具有潜在临床意义的肿瘤治疗方法,它们均由平行的X射线束组成,并允许在肿瘤内递送数千个Gray。我们比较了在体内斑马鱼尾鳍再生过程中,微束(宽25-100μm)和微束(宽200-800μm)对脉管系统,炎症和周围组织变化的影响。微束辐照引发了仅限于再生组织的急性炎症反应。照射后六小时(6 hpi),它被嗜中性粒细胞浸润,并且fli1a(+)血小板细胞在束路径中局部粘附在细胞壁上。成熟的组织不受微束辐射的影响。相反,微型光束照射在6 hpi时有效损伤了未成熟的组织,而在48 hpi时则损伤了成熟的和未成熟的组织。我们证明血管损伤,炎症过程和细胞毒性取决于束宽度和组织成熟的阶段。微型束照射不能区分成熟组织和未成熟组织。相比之下,微束的所有辐照诱导作用都限于迅速生长的未成熟组织,这表明微束辐照可能是一种有前途的肿瘤治疗工具。微型束照射不能区分成熟组织和未成熟组织。相比之下,微束的所有辐照诱导作用都限于迅速生长的未成熟组织,这表明微束辐照可能是一种有前途的肿瘤治疗工具。微型束照射不能区分成熟组织和未成熟组织。相比之下,微束的所有辐照诱导作用都限于迅速生长的未成熟组织,这表明微束辐照可能是一种有前途的肿瘤治疗工具。
更新日期:2016-09-21
中文翻译:

同步辐射在体内诱导中性粒细胞浸润,血小板附着和选择性血管损伤。
我们的目标是可视化体内对微束和微束照射的血管损伤和急性炎症反应。微型束(MRT)和微型束放射疗法(MBRT)是具有潜在临床意义的肿瘤治疗方法,它们均由平行的X射线束组成,并允许在肿瘤内递送数千个Gray。我们比较了在体内斑马鱼尾鳍再生过程中,微束(宽25-100μm)和微束(宽200-800μm)对脉管系统,炎症和周围组织变化的影响。微束辐照引发了仅限于再生组织的急性炎症反应。照射后六小时(6 hpi),它被嗜中性粒细胞浸润,并且fli1a(+)血小板细胞在束路径中局部粘附在细胞壁上。成熟的组织不受微束辐射的影响。相反,微型光束照射在6 hpi时有效损伤了未成熟的组织,而在48 hpi时则损伤了成熟的和未成熟的组织。我们证明血管损伤,炎症过程和细胞毒性取决于束宽度和组织成熟的阶段。微型束照射不能区分成熟组织和未成熟组织。相比之下,微束的所有辐照诱导作用都限于迅速生长的未成熟组织,这表明微束辐照可能是一种有前途的肿瘤治疗工具。微型束照射不能区分成熟组织和未成熟组织。相比之下,微束的所有辐照诱导作用都限于迅速生长的未成熟组织,这表明微束辐照可能是一种有前途的肿瘤治疗工具。微型束照射不能区分成熟组织和未成熟组织。相比之下,微束的所有辐照诱导作用都限于迅速生长的未成熟组织,这表明微束辐照可能是一种有前途的肿瘤治疗工具。






























 京公网安备 11010802027423号
京公网安备 11010802027423号