Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Severity of local inflammation does not impact development of fibrosis in mouse models of intestinal fibrosis.
Scientific Reports ( IF 3.8 ) Pub Date : 2018-Oct-12 , DOI: 10.1038/s41598-018-33452-5 A. Hünerwadel , S. Fagagnini , G. Rogler , C. Lutz , S. U. Jaeger , C. Mamie , B. Weder , P. A. Ruiz , M. Hausmann
Scientific Reports ( IF 3.8 ) Pub Date : 2018-Oct-12 , DOI: 10.1038/s41598-018-33452-5 A. Hünerwadel , S. Fagagnini , G. Rogler , C. Lutz , S. U. Jaeger , C. Mamie , B. Weder , P. A. Ruiz , M. Hausmann
|
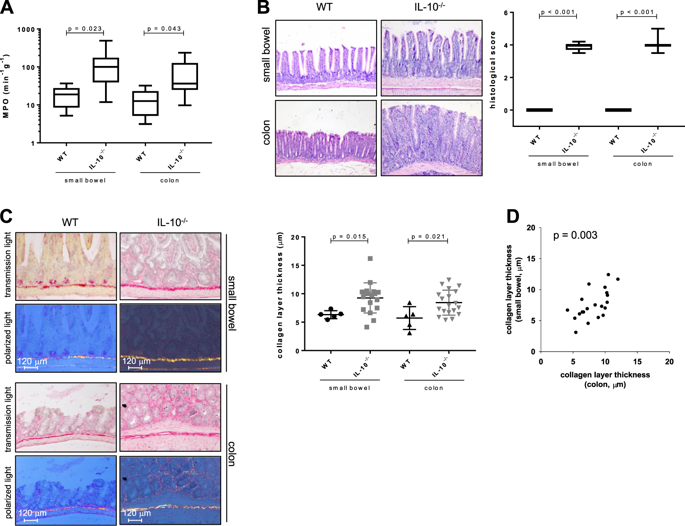
Intestinal fibrosis is thought to be a consequence of excessive tissue repair, and constitutes a common problem in patients with Crohn's disease (CD). While fibrosis seems to require inflammation as a prerequisite it is unclear whether the severity or persistence of inflammation influences the degree of fibrosis. Our aim was to investigate the role of sustained inflammation in fibrogenesis. For the initiation of fibrosis in vivo the models of Il10-/- spontaneous colitis, dextran sodium sulfate (DSS)-induced chronic colitis and heterotopic transplantation were used. In Il10-/- mice, we determined a positive correlation between expression of pro-inflammatory factors (Il1β, Tnf, Ifnγ, Mcp1 and Il6). We also found a positive correlation between the expression of pro-fibrotic factors (Col3a1 Col1a1, Tgfβ and αSma). In contrast, no significant correlation was determined between the expression of pro-inflammatory Tnf and pro-fibrotic αSma, Col1a1, Col3a1, collagen layer thickness and the hydroxyproline (HYP) content. Results from the DSS-induced chronic colitis model confirmed this finding. In the transplantation model for intestinal fibrosis a pronounced increase in Mcp1, inos and Il6 in Il10-/- as compared to WT grafts was observed, indicating more severe inflammation in Il10-/- grafts. However, the increase of collagen over time was virtually identical in both Il10-/- and WT grafts. Severity of inflammation during onset of fibrogenesis did not correlate with collagen deposition. Although inflammation might be a pre-requisite for the initiation of fibrosis our data suggest that it has a minor impact on the progression of fibrosis. Our results suggest that development of fibrosis and inflammation may be disconnected. This may be important for explaining the inefficacy of anti-inflammatory treatments agents in most cases of fibrotic inflammatory bowel diseases (IBD).
中文翻译:

在小鼠肠道纤维化模型中,局部炎症的严重程度不会影响纤维化的发展。
肠道纤维化被认为是过度组织修复的结果,是克罗恩病(CD)患者的普遍问题。虽然纤维化似乎需要炎症作为先决条件,但尚不清楚炎症的严重性或持续性是否会影响纤维化程度。我们的目的是研究持续炎症在纤维发生中的作用。为了在体内引发纤维化,使用了Il10 -/-自发性结肠炎,葡聚糖硫酸钠(DSS)诱导的慢性结肠炎和异位移植的模型。在Il10中-/-在小鼠中,我们确定了促炎因子(Il1β,Tnf,Ifnγ,Mcp1和Il6)的表达之间呈正相关。我们还发现促纤维化因子(Col3a1 Col1a1,Tgfβ和αSma)的表达之间呈正相关。相反,在促炎性Tnf和促纤维化αSma,Col1a1,Col3a1,胶原层厚度和羟脯氨酸(HYP)含量的表达之间未发现显着相关性。DSS诱导的慢性结肠炎模型的结果证实了这一发现。在肠道纤维化的移植模型中,与野生型移植物相比,Il10 -/-中的Mcp1,inos和Il6明显增加,表明Il10 -/-的炎症更加严重移植物。但是,Il10 -/-和WT移植物中胶原蛋白随时间的增加实际上是相同的。纤维化发作期间炎症的严重程度与胶原蛋白沉积无关。尽管炎症可能是引发纤维化的先决条件,但我们的数据表明,炎症对纤维化的进展影响很小。我们的结果表明,纤维化和炎症的发展可能会中断。这对于解释在大多数纤维化性炎症性肠病(IBD)情况下抗炎治疗剂的无效性可能很重要。
更新日期:2018-10-12
中文翻译:

在小鼠肠道纤维化模型中,局部炎症的严重程度不会影响纤维化的发展。
肠道纤维化被认为是过度组织修复的结果,是克罗恩病(CD)患者的普遍问题。虽然纤维化似乎需要炎症作为先决条件,但尚不清楚炎症的严重性或持续性是否会影响纤维化程度。我们的目的是研究持续炎症在纤维发生中的作用。为了在体内引发纤维化,使用了Il10 -/-自发性结肠炎,葡聚糖硫酸钠(DSS)诱导的慢性结肠炎和异位移植的模型。在Il10中-/-在小鼠中,我们确定了促炎因子(Il1β,Tnf,Ifnγ,Mcp1和Il6)的表达之间呈正相关。我们还发现促纤维化因子(Col3a1 Col1a1,Tgfβ和αSma)的表达之间呈正相关。相反,在促炎性Tnf和促纤维化αSma,Col1a1,Col3a1,胶原层厚度和羟脯氨酸(HYP)含量的表达之间未发现显着相关性。DSS诱导的慢性结肠炎模型的结果证实了这一发现。在肠道纤维化的移植模型中,与野生型移植物相比,Il10 -/-中的Mcp1,inos和Il6明显增加,表明Il10 -/-的炎症更加严重移植物。但是,Il10 -/-和WT移植物中胶原蛋白随时间的增加实际上是相同的。纤维化发作期间炎症的严重程度与胶原蛋白沉积无关。尽管炎症可能是引发纤维化的先决条件,但我们的数据表明,炎症对纤维化的进展影响很小。我们的结果表明,纤维化和炎症的发展可能会中断。这对于解释在大多数纤维化性炎症性肠病(IBD)情况下抗炎治疗剂的无效性可能很重要。











































 京公网安备 11010802027423号
京公网安备 11010802027423号