当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Genetic Variants in SGLT1, Glucose Tolerance, and Cardiometabolic Risk
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2018-10-01 , DOI: 10.1016/j.jacc.2018.07.061 Sara B Seidelmann 1 , Elena Feofanova 2 , Bing Yu 2 , Nora Franceschini 3 , Brian Claggett 4 , Mikko Kuokkanen 5 , Hannu Puolijoki 6 , Tapani Ebeling 7 , Markus Perola 5 , Veikko Salomaa 8 , Amil Shah 4 , Josef Coresh 9 , Elizabeth Selvin 9 , Calum A MacRae 4 , Susan Cheng 4 , Eric Boerwinkle 10 , Scott D Solomon 4
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2018-10-01 , DOI: 10.1016/j.jacc.2018.07.061 Sara B Seidelmann 1 , Elena Feofanova 2 , Bing Yu 2 , Nora Franceschini 3 , Brian Claggett 4 , Mikko Kuokkanen 5 , Hannu Puolijoki 6 , Tapani Ebeling 7 , Markus Perola 5 , Veikko Salomaa 8 , Amil Shah 4 , Josef Coresh 9 , Elizabeth Selvin 9 , Calum A MacRae 4 , Susan Cheng 4 , Eric Boerwinkle 10 , Scott D Solomon 4
Affiliation
|
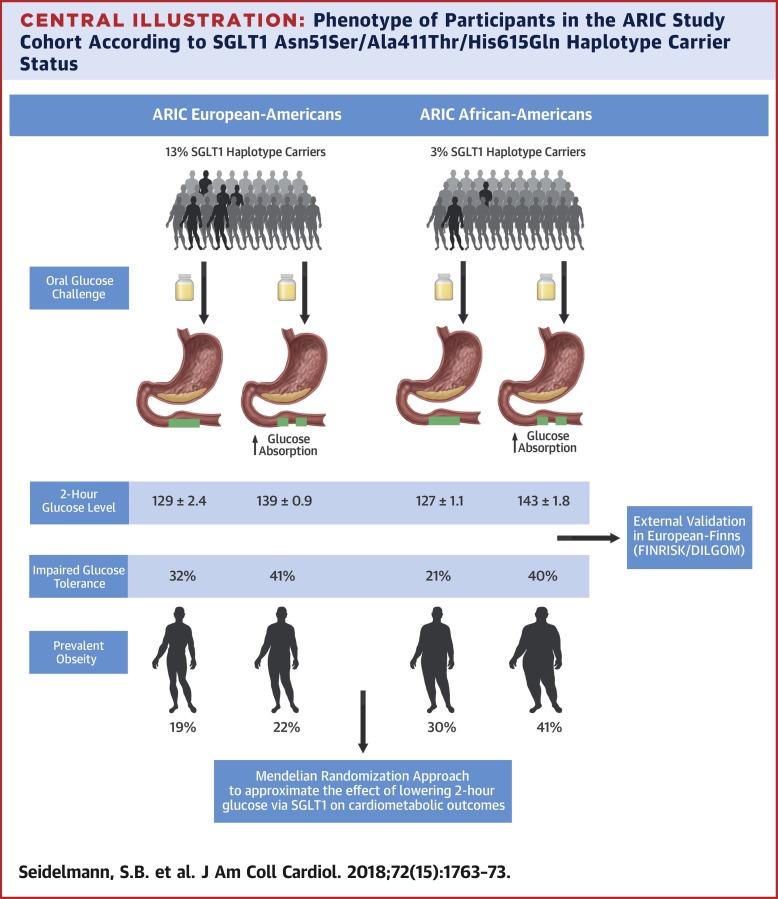
BACKGROUND Loss-of-function mutations in the SGLT1 (sodium/glucose co-transporter-1) gene result in a rare glucose/galactose malabsorption disorder and neonatal death if untreated. In the general population, variants related to intestinal glucose absorption remain uncharacterized. OBJECTIVES The goal of this study was to identify functional SGLT1 gene variants and characterize their clinical consequences. METHODS Whole exome sequencing was performed in the ARIC (Atherosclerosis Risk in Communities) study participants enrolled from 4 U.S. communities. The association of functional, nonsynonymous substitutions in SGLT1 with 2-h oral glucose tolerance test results was determined. Variants related to impaired glucose tolerance were studied, and Mendelian randomization analysis of cardiometabolic outcomes was performed. RESULTS Among 5,687 European-American subjects (mean age 54 ± 6 years; 47% male), those who carried a haplo-type of 3 missense mutations (frequency of 6.7%)—Asn51Ser, Ala411Thr, and His615Gln—had lower 2-h glucose and odds of impaired glucose tolerance than noncarriers (β-coefficient: −8.0; 95% confidence interval [CI]: −12.7 to −3.3; OR: 0.71; 95% CI: 0.59 to 0.86, respectively). The association of the haplotype with oral glucose tolerance test results was consistent in a replication sample of 2,791 African-American subjects (β = −16.3; 95% CI: −36.6 to 4.1; OR: 0.39; 95% CI: 0.17 to 0.91) and an external European-Finnish population sample of 6,784 subjects (β = −3.2; 95% CI: −6.4 to −0.02; OR: 0.81; 95% CI: 0.68 to 0.98). Using a Mendelian randomization approach in the index cohort, the estimated 25-year effect of a reduction of 20 mg/dl in 2-h glucose via SGLT1 inhibition would be reduced prevalent obesity (OR: 0.43; 95% CI: 0.23 to 0.63), incident diabetes (hazard ratio [HR]: 0.58; 95% CI: 0.35 to 0.81), heart failure (HR: 0.53; 95% CI: 0.24 to 0.83), and death (HR: 0.66; 95% CI: 0.42 to 0.90). CONCLUSIONS Functionally damaging missense variants in SGLT1 protect from diet-induced hyperglycemia in multiple populations. Reduced intestinal glucose uptake may protect from long-term cardiometabolic outcomes, providing support for therapies that target SGLT1 function to prevent and treat metabolic condition/ns.
中文翻译:

SGLT1、葡萄糖耐量和心脏代谢风险的遗传变异
背景 SGLT1(钠/葡萄糖协同转运蛋白-1)基因的功能丧失突变如果不治疗,会导致罕见的葡萄糖/半乳糖吸收不良障碍和新生儿死亡。在一般人群中,与肠道葡萄糖吸收相关的变异仍未被表征。目的 本研究的目的是鉴定功能性 SGLT1 基因变异并描述其临床后果。方法 对来自 4 个美国社区的 ARIC(社区动脉粥样硬化风险)研究参与者进行全外显子组测序。确定了 SGLT1 中功能性非同义取代与 2 小时口服葡萄糖耐量测试结果的关联。研究了与糖耐量受损相关的变异,并对心脏代谢结果进行了孟德尔随机分析。结果 在 5,687 名欧洲裔美国受试者中(平均年龄 54 ± 6 岁;47% 为男性),携带 3 个错义突变单倍体型(频率为 6.7%)——Asn51Ser、Ala411Thr 和 His615Gln——的受试者 2-h 较低与非携带者相比,葡萄糖和糖耐量受损的几率更高(β系数:-8.0;95%置信区间[CI]:-12.7至-3.3;OR:0.71;95% CI:0.59至0.86)。单倍型与口服葡萄糖耐量测试结果的关联在 2,791 名非裔美国受试者的复制样本中是一致的(β = -16.3;95% CI:-36.6 至 4.1;OR:0.39;95% CI:0.17 至 0.91)以及 6,784 名受试者的欧洲-芬兰外部人口样本(β = -3.2;95% CI:-6.4 至 -0.02;OR:0.81;95% CI:0.68 至 0.98)。在指数队列中使用孟德尔随机化方法,通过 SGLT1 抑制将 2 小时血糖降低 20 mg/dl 的估计 25 年效果将减少普遍肥胖(OR:0.43;95% CI:0.23 至 0.63) 、糖尿病事件(风险比 [HR]:0.58;95% CI:0.35 至 0.81)、心力衰竭(HR:0.53;95% CI:0.24 至 0.83)和死亡(HR:0.66;95% CI:0.42 至0.90)。结论 SGLT1 中具有功能性破坏性的错义变异可以保护多个人群免受饮食诱发的高血糖症。减少肠道葡萄糖摄取可以防止长期心脏代谢结果,为针对 SGLT1 功能的疗法提供支持,以预防和治疗代谢疾病。
更新日期:2018-10-01
中文翻译:

SGLT1、葡萄糖耐量和心脏代谢风险的遗传变异
背景 SGLT1(钠/葡萄糖协同转运蛋白-1)基因的功能丧失突变如果不治疗,会导致罕见的葡萄糖/半乳糖吸收不良障碍和新生儿死亡。在一般人群中,与肠道葡萄糖吸收相关的变异仍未被表征。目的 本研究的目的是鉴定功能性 SGLT1 基因变异并描述其临床后果。方法 对来自 4 个美国社区的 ARIC(社区动脉粥样硬化风险)研究参与者进行全外显子组测序。确定了 SGLT1 中功能性非同义取代与 2 小时口服葡萄糖耐量测试结果的关联。研究了与糖耐量受损相关的变异,并对心脏代谢结果进行了孟德尔随机分析。结果 在 5,687 名欧洲裔美国受试者中(平均年龄 54 ± 6 岁;47% 为男性),携带 3 个错义突变单倍体型(频率为 6.7%)——Asn51Ser、Ala411Thr 和 His615Gln——的受试者 2-h 较低与非携带者相比,葡萄糖和糖耐量受损的几率更高(β系数:-8.0;95%置信区间[CI]:-12.7至-3.3;OR:0.71;95% CI:0.59至0.86)。单倍型与口服葡萄糖耐量测试结果的关联在 2,791 名非裔美国受试者的复制样本中是一致的(β = -16.3;95% CI:-36.6 至 4.1;OR:0.39;95% CI:0.17 至 0.91)以及 6,784 名受试者的欧洲-芬兰外部人口样本(β = -3.2;95% CI:-6.4 至 -0.02;OR:0.81;95% CI:0.68 至 0.98)。在指数队列中使用孟德尔随机化方法,通过 SGLT1 抑制将 2 小时血糖降低 20 mg/dl 的估计 25 年效果将减少普遍肥胖(OR:0.43;95% CI:0.23 至 0.63) 、糖尿病事件(风险比 [HR]:0.58;95% CI:0.35 至 0.81)、心力衰竭(HR:0.53;95% CI:0.24 至 0.83)和死亡(HR:0.66;95% CI:0.42 至0.90)。结论 SGLT1 中具有功能性破坏性的错义变异可以保护多个人群免受饮食诱发的高血糖症。减少肠道葡萄糖摄取可以防止长期心脏代谢结果,为针对 SGLT1 功能的疗法提供支持,以预防和治疗代谢疾病。

































 京公网安备 11010802027423号
京公网安备 11010802027423号