Prostate Cancer and Prostatic Diseases ( IF 5.1 ) Pub Date : 2018-08-21 , DOI: 10.1038/s41391-018-0079-0 E. David Crawford , Axel Heidenreich , Nathan Lawrentschuk , Bertrand Tombal , Antonio C. L. Pompeo , Arturo Mendoza-Valdes , Kurt Miller , Frans M. J. Debruyne , Laurence Klotz
|
Background
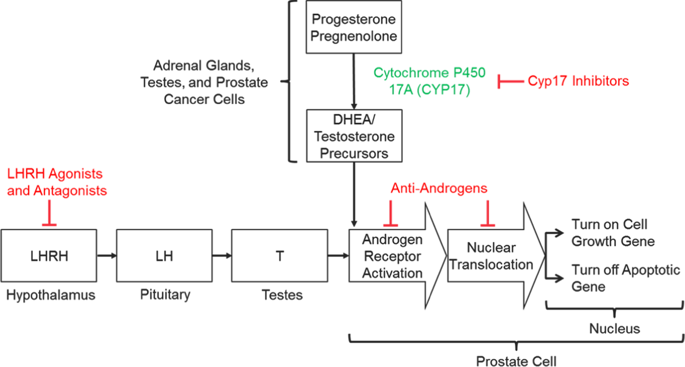
Androgen deprivation therapy (ADT) is foundational in the management of advanced prostate cancer (PCa) and has benefitted from a recent explosion in scientific advances. These include approval of new therapies that suppress testosterone (T) levels or inactivate its function, improvements in diagnostic and assay technologies, identification of lower therapeutic targets for T, discovery of the relevance of germline genetic mutations and identification of the benefits of sequential and combination therapies.
Methods
This review discusses the clinical profiles of the most up-to-date options for ADT, best practices for managing patients with advanced PCa and future directions in therapy.
Results and conclusions
Modern assay technologies reveal that bilateral orchiectomy results in a serum T level of approximately 15 ng/dL as compared to the historical definition of castration of T < 50 ng/dL. Evidence shows that lowering T levels to <20 ng/dL improves patient survival and delays disease progression. Routine monitoring of T in addition to prostate-specific antigen throughout treatment is important to ensure continuing efficacy of T suppression. New drugs that inhibit androgen signaling in combination with traditional ADT suppress T activity to near zero and have significantly improved patient survival. When personalizing ADT regimens physicians should consider a number of factors including initiation and duration of ADT, monitoring of T levels and PSA, the possibility of switching monotherapies if a patient does not achieve adequate T suppression, and consideration of intermittent vs. continuous ADT according to patients’ lifestyles, comorbidities, risk factors and tolerance to treatment.
中文翻译:

前列腺癌男性的雄激素靶向治疗:不断发展的实践和未来的考虑
背景
雄激素剥夺疗法(ADT)是晚期前列腺癌(PCa)治疗的基础,并得益于最近科学进展的激增。这些措施包括批准抑制睾丸激素(T)水平或使其功能失活的新疗法,诊断和测定技术的改进,确定T的较低治疗靶标,发现种系遗传突变的相关性以及确定序贯和组合的益处疗法。
方法
这篇综述讨论了ADT的最新选择的临床概况,治疗晚期PCa的患者的最佳实践以及治疗的未来方向。
结果与结论
现代分析技术表明,与以往的of割<50 ng / dL的历史定义相比,双侧睾丸切除术的血清T水平约为15 ng / dL。有证据表明,将T水平降低至<20 ng / dL可以改善患者的存活率并延缓疾病的进展。在整个治疗过程中,除了前列腺特异性抗原外,对T进行例行监测对于确保T抑制的持续疗效也很重要。与传统ADT结合使用的抑制雄激素信号的新药可将T活性抑制到接近零,并显着提高了患者的生存率。当个性化ADT方案时,医生应考虑许多因素,包括ADT的开始和持续时间,T水平和PSA的监测,如果患者未能获得足够的T抑制而改用单一疗法的可能性,































 京公网安备 11010802027423号
京公网安备 11010802027423号