Nutrition & Diabetes ( IF 4.6 ) Pub Date : 2018-06-01 , DOI: 10.1038/s41387-018-0047-8 Kristine Færch , Marjan Alssema , David J. Mela , Rikke Borg , Dorte Vistisen
|
Background/objective
There is substantial interest in dietary approaches to reducing postprandial glucose (PPG) responses, but the quantitative contribution of PPG to longer-term glycemic control (reflected in glycated hemoglobin, HbA1c) in the general population is not known. This study quantified the associations of preprandial glucose exposure, PPG exposure, and glycemic variability with HbA1c and estimated the explained variance in HbA1c in individuals with and without type 2 diabetes (T2D).
Subjects/methods
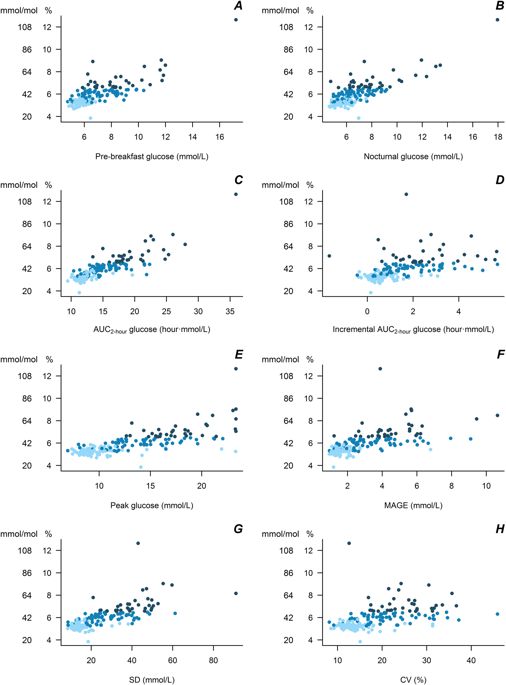
Participants in the A1c-Derived Average Glucose (ADAG) study without T2D (n = 77) or with non-insulin-treated T2D and HbA1c<6.5% (T2DHbA1c < 6.5%, n = 63) or HbA1c ≥ 6.5% (T2DHbA1c ≥ 6.5%, n = 34) were included in this analysis. Indices of preprandial glucose, PPG, and glycemic variability were calculated from continuous glucose monitoring during four periods over 12 weeks prior to HbA1c measurement. In linear regression models, we estimated the associations of the glycemic exposures with HbA1c and calculated the proportion of variance in HbA1c explained by glycemic and non-glycemic factors (age, sex, body mass index, and ethnicity).
Results
The factors in the analysis explained 35% of the variance in HbA1c in non-diabetic individuals, 49% in T2DHbA1c < 6.5%, and 78% in T2DHbA1c ≥ 6.5%. In non-diabetic individuals PPG exposure was associated with HbA1c in confounder-adjusted analyses (P < 0.05). In the T2DHbA1c < 6.5% group, all glycemic measures were associated with HbA1c (P < 0.05); preprandial glucose and PPG accounted for 14 and 18%, respectively, of the explained variation. In T2DHbA1c ≥ 6.5%, these glycemic exposures accounted for more than 50% of the variation in HbA1c and with equal relative contributions.
Conclusions
Among the glycemic exposures, PPG exposure was most strongly predictive of HbA1c in non-diabetic individuals, suggesting that interventions targeting lowering of the PPG response may be beneficial for long-term glycemic maintenance. In T2D, preprandial glucose and PPG exposure contributed equally to HbA1c.
中文翻译:

糖尿病患者和非糖尿病患者餐前和餐后葡萄糖暴露,血糖变异性和非血糖因素对HbA 1c的相对贡献
背景/目标
降低饮食中餐后葡萄糖(PPG)反应的饮食方法引起了人们的极大兴趣,但是在一般人群中PPG对长期血糖控制(反映在糖化血红蛋白HbA 1c中)的定量贡献尚不明确。这项研究量化了餐前血糖暴露,PPG暴露和血糖变异性与HbA 1c的关联,并估计了患有和不患有2型糖尿病(T2D)的个体中HbA 1c的解释差异。
主题/方法
参与者A1c的衍生的平均葡萄糖(ADAG)研究而不T2D(Ñ = 77)或与非胰岛素治疗的T2D和HBA 1c的<6.5%(T2D的HbA1c <6.5% ,Ñ = 63)或HBA 1C ≥6.5% (T2D HbA1c≥6.5%,n = 34)包括在该分析中。餐前血糖,PPG和血糖变异性的指标是通过在HbA 1c测量之前的12周内的四个时段内连续监测血糖来计算的。在线性回归模型中,我们估计了血糖暴露与HbA 1c的关联,并计算了HbA 1c中的方差比例 由血糖和非血糖因素(年龄,性别,体重指数和种族)解释。
结果
分析中的因素解释了非糖尿病个体中HbA 1c变异的35%,T2D HbA1c <6.5%的49%和T2D HbA1c≥6.5%的78 %。在混杂因素校正分析中,非糖尿病患者中PPG暴露与HbA 1c相关(P <0.05)。在T2D HbA1c <6.5%组中,所有血糖测量值均与HbA 1c相关(P <0.05);餐前葡萄糖和PPG分别占所解释变异的14%和18%。在T2D HbA1c≥6.5%中,这些血糖暴露占HbA 1c变化的50%以上,并且具有相等的相对贡献。
结论
在血糖暴露中,PPG暴露最能预测非糖尿病患者的HbA 1c,这表明针对降低PPG反应的干预措施可能有益于长期血糖维持。在T2D中,餐前血糖和PPG暴露对HbA 1c的贡献相同。

































 京公网安备 11010802027423号
京公网安备 11010802027423号