当前位置:
X-MOL 学术
›
Modern Pathol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
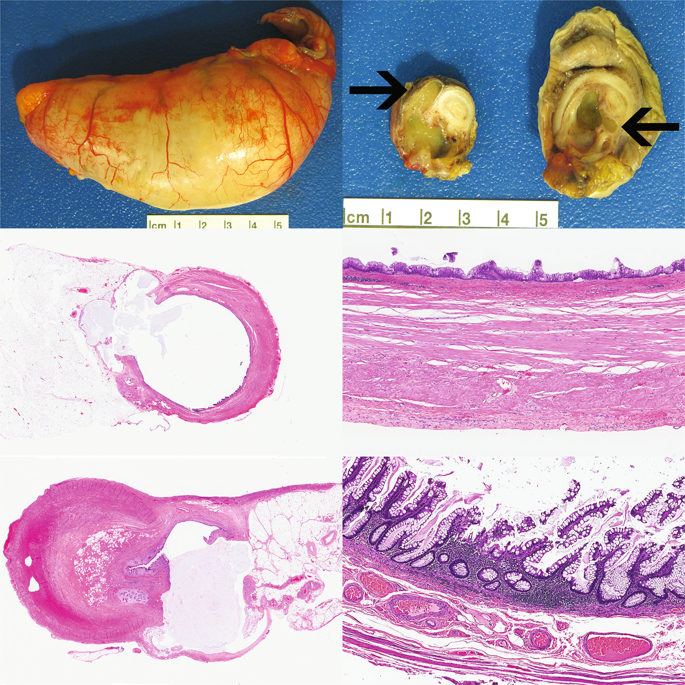
Post-inflammatory mucosal hyperplasia and appendiceal diverticula simulate features of low-grade appendiceal mucinous neoplasms.
Modern Pathology ( IF 7.1 ) Pub Date : 2019-12-19 , DOI: 10.1038/s41379-019-0435-1 Erika Hissong 1 , Tamara Goncharuk 1 , Wei Song 1 , Rhonda K Yantiss 1
Modern Pathology ( IF 7.1 ) Pub Date : 2019-12-19 , DOI: 10.1038/s41379-019-0435-1 Erika Hissong 1 , Tamara Goncharuk 1 , Wei Song 1 , Rhonda K Yantiss 1
Affiliation
|
Post-inflammatory mucosal hyperplasia and appendiceal diverticulosis simulate mucinous neoplasms, causing diagnostic confusion. Distinction between neoplasia and its mimics is particularly important since many authorities now consider all appendiceal mucinous neoplasms to be potentially malignant. The purpose of this study was to identify clinicopathologic and molecular features that may distinguish appendiceal mucinous neoplasms from non-neoplastic mimics. We retrospectively identified 92 mucinous lesions confined to the right lower quadrant, including 55 non-neoplastic examples of mucosal hyperplasia and/or diverticulosis and 37 low-grade neoplasms. Presenting symptoms, radiographic findings, appendiceal diameter, appearances of the lamina propria, non-neoplastic crypts, and epithelium, as well as mural changes were recorded. Twenty non-neoplastic lesions were subjected to KRAS mutational testing. Non-neoplastic appendices were smaller (p < 0.05) and more likely to present with symptoms of appendicitis (p < 0.05) than neoplasms. While post-inflammatory mucosal hyperplasia and diverticula often showed goblet cell-rich epithelium, extruded mucin pools, and patchy mural alterations with fibrosis, they always contained non-neoplastic crypts lined by mixed epithelial cell types and separated by lamina propria with predominantly preserved wall architecture. On the other hand, mucinous neoplasms lacked normal crypts (p < 0.05) and showed decreased lamina propria (p < 0.05) with diffusely thickened muscularis mucosae and lymphoid atrophy. Six (30%) non-neoplastic lesions contained KRAS mutations, particularly those containing goblet cell-rich hyperplastic epithelium. We conclude that distinction between neoplastic and non-neoplastic mucinous appendiceal lesions requires recognition of key morphologic features; KRAS mutational testing is an unreliable biomarker that cannot be used to assess biologic risk or confirm a diagnosis of neoplasia.
中文翻译:

炎症后粘膜增生和阑尾憩室类似于低级别阑尾粘液性肿瘤的特征。
炎症后粘膜增生和阑尾憩室病类似于粘液性肿瘤,导致诊断混乱。区分肿瘤及其类似物尤为重要,因为许多权威人士现在认为所有阑尾粘液性肿瘤都可能是恶性的。本研究的目的是确定可区分阑尾粘液性肿瘤和非肿瘤样肿瘤的临床病理学和分子特征。我们回顾性地确定了 92 个局限于右下腹的粘液性病变,包括 55 个粘膜增生和/或憩室病的非肿瘤病例和 37 个低度恶性肿瘤。记录表现症状、影像学表现、阑尾直径、固有层外观、非肿瘤性隐窝和上皮,以及壁变化。对 20 个非肿瘤性病变进行了 KRAS 突变检测。与肿瘤相比,非肿瘤性阑尾更小 (p < 0.05),并且更可能出现阑尾炎症状 (p < 0.05)。虽然炎症后粘膜增生和憩室通常显示富含杯状细胞的上皮、挤出的粘蛋白池和伴有纤维化的斑片状壁改变,但它们总是包含非肿瘤性隐窝,内衬混合上皮细胞类型,由固有层分隔,壁结构主要保留. 另一方面,粘液性肿瘤缺乏正常的隐窝 (p < 0.05) 并显示固有层减少 (p < 0.05),伴有弥漫性增厚的粘膜肌层和淋巴萎缩。六个 (30%) 非肿瘤性病变包含 KRAS 突变,特别是那些含有富含杯状细胞的增生性上皮细胞。我们得出结论,区分肿瘤性和非肿瘤性粘液性阑尾病变需要识别关键的形态学特征;KRAS 突变检测是一种不可靠的生物标志物,不能用于评估生物学风险或确认肿瘤的诊断。
更新日期:2019-12-20
中文翻译:

炎症后粘膜增生和阑尾憩室类似于低级别阑尾粘液性肿瘤的特征。
炎症后粘膜增生和阑尾憩室病类似于粘液性肿瘤,导致诊断混乱。区分肿瘤及其类似物尤为重要,因为许多权威人士现在认为所有阑尾粘液性肿瘤都可能是恶性的。本研究的目的是确定可区分阑尾粘液性肿瘤和非肿瘤样肿瘤的临床病理学和分子特征。我们回顾性地确定了 92 个局限于右下腹的粘液性病变,包括 55 个粘膜增生和/或憩室病的非肿瘤病例和 37 个低度恶性肿瘤。记录表现症状、影像学表现、阑尾直径、固有层外观、非肿瘤性隐窝和上皮,以及壁变化。对 20 个非肿瘤性病变进行了 KRAS 突变检测。与肿瘤相比,非肿瘤性阑尾更小 (p < 0.05),并且更可能出现阑尾炎症状 (p < 0.05)。虽然炎症后粘膜增生和憩室通常显示富含杯状细胞的上皮、挤出的粘蛋白池和伴有纤维化的斑片状壁改变,但它们总是包含非肿瘤性隐窝,内衬混合上皮细胞类型,由固有层分隔,壁结构主要保留. 另一方面,粘液性肿瘤缺乏正常的隐窝 (p < 0.05) 并显示固有层减少 (p < 0.05),伴有弥漫性增厚的粘膜肌层和淋巴萎缩。六个 (30%) 非肿瘤性病变包含 KRAS 突变,特别是那些含有富含杯状细胞的增生性上皮细胞。我们得出结论,区分肿瘤性和非肿瘤性粘液性阑尾病变需要识别关键的形态学特征;KRAS 突变检测是一种不可靠的生物标志物,不能用于评估生物学风险或确认肿瘤的诊断。






























 京公网安备 11010802027423号
京公网安备 11010802027423号