Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
The human capsular bag model of posterior capsule opacification
Eye ( IF 2.8 ) Pub Date : 2019-11-19 , DOI: 10.1038/s41433-019-0680-z I Michael Wormstone 1
Eye ( IF 2.8 ) Pub Date : 2019-11-19 , DOI: 10.1038/s41433-019-0680-z I Michael Wormstone 1
Affiliation
|
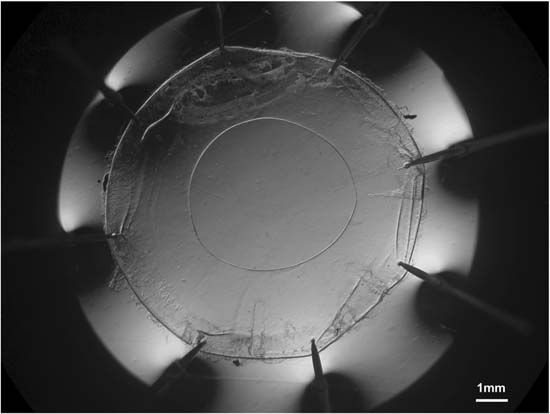
Posterior capsule opacification (PCO) is the most common complication following cataract surgery and affects millions of patients. PCO is a consequence of surgical injury promoting a wound-healing response. Following surgery, residual lens epithelial cells grow on acellular regions of the lens capsule, including the central posterior capsule. These cells can undergo fibrotic changes, such that cell transdifferentiation to myofibroblasts, matrix deposition and matrix contraction can occur, which contribute to light scatter and the need for further corrective Nd:YAG laser capsulotomy in many patients. It is therefore of great importance to better understand how PCO develops and determine better approaches to manage the condition. To achieve this, experimental systems are required, and many are available to study PCO. While there may be a number of common features associated with PCO in different species, the mechanisms governing the condition can differ. Consequently, where possible, human systems should be employed. The human capsular bag model was established in a laboratory setting on donor eyes. A capsulorhexis is performed to create an opening in the anterior capsule followed by removal of the lens fibre mass. Residual fibre cells can be removed by irrigation/aspiration and if required, an intraocular lens can be implanted. The capsular bag is isolated from the eye and transferred to a dish for culture. The human capsular bag model has played an important role in understanding the biological processes driving PCO and enables evaluation of surgical approaches, IOLs and putative therapeutic agents to better manage PCO. 后囊浑浊 (PCO) 是白内障术后最常见的并发症, 且影响着数百万患者。PCO是手术损伤后促进伤口发生愈合反应的结果。术后残余的晶状体上皮细胞在晶状体囊无细胞区域生长, 包括后囊中央区。这些细胞可发生纤维化改变, 从而使上皮细胞转分化为肌成纤维细胞, 并可能发生基质沉积和基质收缩, 这将会导致晶状体的光散射, 使许多病人需要更进一步的矫正措施—Nd: YAG激光后囊切开术。因此, 更全面地了解PCO是如何发生发展的和采取更好的措施来处理这些情况是极其重要的。为了实现这个实验, 系统是必须的, 且许多都可用于PCO的研究。虽然在不同物种中可能有许多与PCO相关的共同特点, 但控制情况的机制可以不同。因此在可能的情况下, 应采用人类 (真人的) 系统。在实验室条件下建立了供眼人类囊袋模型。实施撕囊术在前囊形成一个开口, 然后去除晶状体纤维团块。残余的纤维细胞可以通过冲洗或抽吸去除, 如果需要的话, 可植入眼内人工晶状体。将囊袋从眼中分离出来, 转移至培养皿内培养。人类囊袋模型在理解PCO生物学过程中起重要作用, 并使手术方法, 人工晶状体和假定的治疗药物的评估能更好地管理PCO。
中文翻译:

人体后囊膜混浊囊袋模型
Posterior capsule opacification (PCO) is the most common complication following cataract surgery and affects millions of patients. PCO is a consequence of surgical injury promoting a wound-healing response. Following surgery, residual lens epithelial cells grow on acellular regions of the lens capsule, including the central posterior capsule. These cells can undergo fibrotic changes, such that cell transdifferentiation to myofibroblasts, matrix deposition and matrix contraction can occur, which contribute to light scatter and the need for further corrective Nd:YAG laser capsulotomy in many patients. It is therefore of great importance to better understand how PCO develops and determine better approaches to manage the condition. To achieve this, experimental systems are required, and many are available to study PCO. While there may be a number of common features associated with PCO in different species, the mechanisms governing the condition can differ. Consequently, where possible, human systems should be employed. The human capsular bag model was established in a laboratory setting on donor eyes. A capsulorhexis is performed to create an opening in the anterior capsule followed by removal of the lens fibre mass. Residual fibre cells can be removed by irrigation/aspiration and if required, an intraocular lens can be implanted. The capsular bag is isolated from the eye and transferred to a dish for culture. The human capsular bag model has played an important role in understanding the biological processes driving PCO and enables evaluation of surgical approaches, IOLs and putative therapeutic agents to better manage PCO. 后囊浑浊 (PCO) 是白内障术后最常见的并发症, 且影响着数百万患者。PCO是手术损伤后促进伤口发生愈合反应的结果。术后残余的晶状体上皮细胞在晶状体囊无细胞区域生长, 包括后囊中央区。这些细胞可发生纤维化改变, 从而使上皮细胞转分化为肌成纤维细胞, 并可能发生基质沉积和基质收缩, 这将会导致晶状体的光散射, 使许多病人需要更进一步的矫正措施—Nd: YAG激光后囊切开术。因此, 更全面地了解PCO是如何发生发展的和采取更好的措施来处理这些情况是极其重要的。为了实现这个实验, 系统是必须的, 且许多都可用于PCO的研究。虽然在不同物种中可能有许多与PCO相关的共同特点, 但控制情况的机制可以不同。因此在可能的情况下, 应采用人类 (真人的) 系统。在实验室条件下建立了供眼人类囊袋模型。实施撕囊术在前囊形成一个开口, 然后去除晶状体纤维团块。残余的纤维细胞可以通过冲洗或抽吸去除, 如果需要的话, 可植入眼内人工晶状体。将囊袋从眼中分离出来, 转移至培养皿内培养。人类囊袋模型在理解PCO生物学过程中起重要作用, 并使手术方法, 人工晶状体和假定的治疗药物的评估能更好地管理PCO。
更新日期:2019-11-19
中文翻译:

人体后囊膜混浊囊袋模型
Posterior capsule opacification (PCO) is the most common complication following cataract surgery and affects millions of patients. PCO is a consequence of surgical injury promoting a wound-healing response. Following surgery, residual lens epithelial cells grow on acellular regions of the lens capsule, including the central posterior capsule. These cells can undergo fibrotic changes, such that cell transdifferentiation to myofibroblasts, matrix deposition and matrix contraction can occur, which contribute to light scatter and the need for further corrective Nd:YAG laser capsulotomy in many patients. It is therefore of great importance to better understand how PCO develops and determine better approaches to manage the condition. To achieve this, experimental systems are required, and many are available to study PCO. While there may be a number of common features associated with PCO in different species, the mechanisms governing the condition can differ. Consequently, where possible, human systems should be employed. The human capsular bag model was established in a laboratory setting on donor eyes. A capsulorhexis is performed to create an opening in the anterior capsule followed by removal of the lens fibre mass. Residual fibre cells can be removed by irrigation/aspiration and if required, an intraocular lens can be implanted. The capsular bag is isolated from the eye and transferred to a dish for culture. The human capsular bag model has played an important role in understanding the biological processes driving PCO and enables evaluation of surgical approaches, IOLs and putative therapeutic agents to better manage PCO. 后囊浑浊 (PCO) 是白内障术后最常见的并发症, 且影响着数百万患者。PCO是手术损伤后促进伤口发生愈合反应的结果。术后残余的晶状体上皮细胞在晶状体囊无细胞区域生长, 包括后囊中央区。这些细胞可发生纤维化改变, 从而使上皮细胞转分化为肌成纤维细胞, 并可能发生基质沉积和基质收缩, 这将会导致晶状体的光散射, 使许多病人需要更进一步的矫正措施—Nd: YAG激光后囊切开术。因此, 更全面地了解PCO是如何发生发展的和采取更好的措施来处理这些情况是极其重要的。为了实现这个实验, 系统是必须的, 且许多都可用于PCO的研究。虽然在不同物种中可能有许多与PCO相关的共同特点, 但控制情况的机制可以不同。因此在可能的情况下, 应采用人类 (真人的) 系统。在实验室条件下建立了供眼人类囊袋模型。实施撕囊术在前囊形成一个开口, 然后去除晶状体纤维团块。残余的纤维细胞可以通过冲洗或抽吸去除, 如果需要的话, 可植入眼内人工晶状体。将囊袋从眼中分离出来, 转移至培养皿内培养。人类囊袋模型在理解PCO生物学过程中起重要作用, 并使手术方法, 人工晶状体和假定的治疗药物的评估能更好地管理PCO。































 京公网安备 11010802027423号
京公网安备 11010802027423号