Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Antimalarial Quinoline Drugs Inhibit β-Hematin and Increase Free Hemin Catalyzing Peroxidative Reactions and Inhibition of Cysteine Proteases.
Scientific Reports ( IF 3.8 ) Pub Date : 2019-10-28 , DOI: 10.1038/s41598-019-51604-z Tomás Herraiz 1 , Hugo Guillén 1 , Diana González-Peña 1 , Vicente J Arán 2
Scientific Reports ( IF 3.8 ) Pub Date : 2019-10-28 , DOI: 10.1038/s41598-019-51604-z Tomás Herraiz 1 , Hugo Guillén 1 , Diana González-Peña 1 , Vicente J Arán 2
Affiliation
|
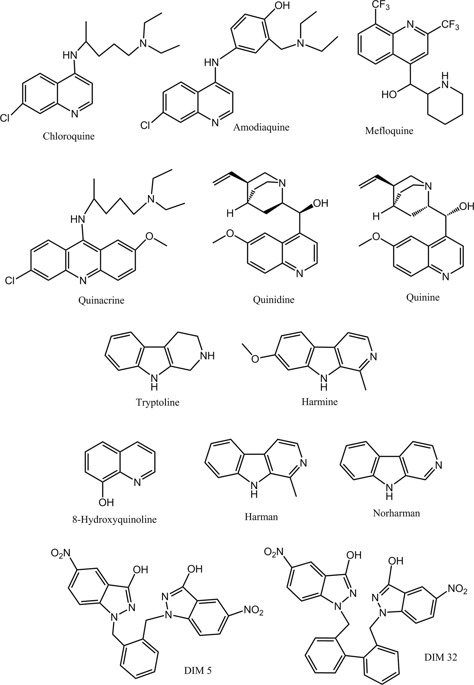
Malaria caused by Plasmodium affects millions people worldwide. Plasmodium consumes hemoglobin during its intraerythrocytic stage leaving toxic heme. Parasite detoxifies free heme through formation of hemozoin (β-hematin) pigment. Proteolysis of hemoglobin and formation of hemozoin are two main targets for antimalarial drugs. Quinoline antimarial drugs and analogs (β-carbolines or nitroindazoles) were studied as inhibitors of β-hematin formation. The most potent inhibitors were quinacrine, chloroquine, and amodiaquine followed by quinidine, mefloquine and quinine whereas 8-hydroxyquinoline and β-carbolines had no effect. Compounds that inhibited β-hematin increased free hemin that promoted peroxidative reactions as determined with TMB and ABTS substrates. Hemin-catalyzed peroxidative reactions were potentiated in presence of proteins (i.e. globin or BSA) while antioxidants and peroxidase inhibitors decreased peroxidation. Free hemin increased by chloroquine action promoted oxidative reactions resulting in inhibition of proteolysis by three cysteine proteases: papain, ficin and cathepsin B. Glutathione reversed inhibition of proteolysis. These results show that active quinolines inhibit hemozoin and increase free hemin which in presence of H2O2 that abounds in parasite digestive vacuole catalyzes peroxidative reactions and inhibition of cysteine proteases. This work suggests a link between the action of quinoline drugs with biochemical processes of peroxidation and inhibition of proteolysis.
中文翻译:

抗疟喹啉药物可抑制 β-血红素并增加催化过氧化反应的游离血红素并抑制半胱氨酸蛋白酶。
由疟原虫引起的疟疾影响着全世界数百万人。疟原虫在红细胞内阶段消耗血红蛋白,留下有毒的血红素。寄生虫通过形成疟原虫色素(β-血红素)来解毒游离血红素。血红蛋白的蛋白水解和疟原虫色素的形成是抗疟药物的两个主要目标。研究了喹啉抗婚药和类似物(β-咔啉或硝基吲唑)作为 β-血红素形成的抑制剂。最有效的抑制剂是奎纳克林、氯喹和阿莫地喹,其次是奎尼丁、甲氟喹和奎宁,而 8-羟基喹啉和 β-咔啉则没有作用。抑制 β-血红素的化合物会增加游离血红素,从而促进过氧化反应(根据 TMB 和 ABTS 底物测定)。氯化血红素催化的过氧化反应在蛋白质(即珠蛋白或 BSA)存在下增强,而抗氧化剂和过氧化物酶抑制剂则减少过氧化反应。氯喹作用增加的游离血红素促进了氧化反应,导致三种半胱氨酸蛋白酶(木瓜蛋白酶、无花果蛋白酶和组织蛋白酶 B)的蛋白水解抑制。谷胱甘肽逆转了蛋白水解的抑制。这些结果表明,活性喹啉抑制疟原虫色素并增加游离氯化血红素,在寄生虫消化液泡中富含的H2O2存在下,游离氯化血红素可催化过氧化反应并抑制半胱氨酸蛋白酶。这项工作表明喹啉药物的作用与过氧化和抑制蛋白水解的生化过程之间存在联系。
更新日期:2019-10-28
中文翻译:

抗疟喹啉药物可抑制 β-血红素并增加催化过氧化反应的游离血红素并抑制半胱氨酸蛋白酶。
由疟原虫引起的疟疾影响着全世界数百万人。疟原虫在红细胞内阶段消耗血红蛋白,留下有毒的血红素。寄生虫通过形成疟原虫色素(β-血红素)来解毒游离血红素。血红蛋白的蛋白水解和疟原虫色素的形成是抗疟药物的两个主要目标。研究了喹啉抗婚药和类似物(β-咔啉或硝基吲唑)作为 β-血红素形成的抑制剂。最有效的抑制剂是奎纳克林、氯喹和阿莫地喹,其次是奎尼丁、甲氟喹和奎宁,而 8-羟基喹啉和 β-咔啉则没有作用。抑制 β-血红素的化合物会增加游离血红素,从而促进过氧化反应(根据 TMB 和 ABTS 底物测定)。氯化血红素催化的过氧化反应在蛋白质(即珠蛋白或 BSA)存在下增强,而抗氧化剂和过氧化物酶抑制剂则减少过氧化反应。氯喹作用增加的游离血红素促进了氧化反应,导致三种半胱氨酸蛋白酶(木瓜蛋白酶、无花果蛋白酶和组织蛋白酶 B)的蛋白水解抑制。谷胱甘肽逆转了蛋白水解的抑制。这些结果表明,活性喹啉抑制疟原虫色素并增加游离氯化血红素,在寄生虫消化液泡中富含的H2O2存在下,游离氯化血红素可催化过氧化反应并抑制半胱氨酸蛋白酶。这项工作表明喹啉药物的作用与过氧化和抑制蛋白水解的生化过程之间存在联系。































 京公网安备 11010802027423号
京公网安备 11010802027423号