Journal of Human Hypertension ( IF 2.7 ) Pub Date : 2019-10-17 , DOI: 10.1038/s41371-019-0270-3 Federica Di Gennaro 1 , Cinzia D'Amato 1 , Roberto Morganti 1 , Carla Greco 1 , Susanna Longo 1 , Diana Corradini 1 , Davide Lauro 1 , Vincenza Spallone 1
|
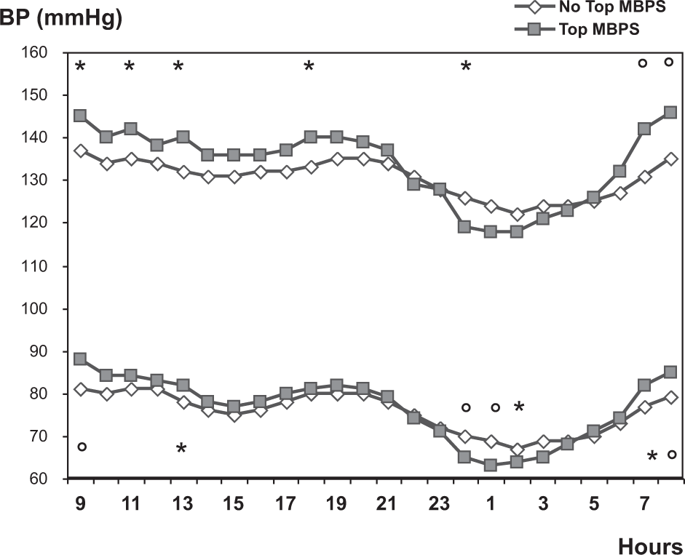
Although vascular and autonomic nervous system have been involved in the regulation of morning surge in blood pressure (MBPS), data on clinical correlates of MBPS in diabetic population are scarce, in particular with regard to diabetic complications. This study was aimed at investigating predictors and correlates of MBPS in diabetes. In a cross-sectional study including 167 patients with diabetes (age 58.5 ± 11.1 years, duration 15.9 ± 12.1 years), clinical variables, diabetic and neuropathic complications, and MBPS (using 24-h ambulatory blood pressure monitoring) were measured. The upper quartile of MBPS (>30.5 mmHg) was associated with higher values of waist circumference (P = 0.027), triglycerides (P = 0.021), and Michigan Diabetic Neuropathy Score (P = 0.042), with lower HDL cholesterol (P = 0.030), and with the presence of cardiovascular autonomic neuropathy (CAN) (P = 0.016) and peripheral vascular disease (PVD) (P < 0.0001). In a logistic regression analysis, PVD (odds ratio: 10.2, P = 0.001), CAN (odds ratio: 6.09, P = 0.016), and diastolic blood pressure (BP) (odds ratio: 1.06, P = 0.022) predicted MBPS upper quartile (r2 = 0.20, P = 0.0005). In a multiple regression analysis, PVD (P = 0.002) and diastolic BP (P = 0.003) were the only determinants of MBPS (r2 = 0.20). MBPS upper quartile was associated with BP dipping (systolic BP day–night reduction > 10%) (P = 0.012), and MBPS was positively related to systolic (rho = 0.41, P < 0.0001) and diastolic BP day–night reduction. In conclusion, metabolic syndrome stigmata, diastolic BP, CAN and PVD are the main predictors of MBPS in the diabetic population. Excessive MBPS and nondipping are not concurrent 24-h BP alterations. Autonomic dysfunction might exert an exacerbating effect on MBPS phenomenon.
中文翻译:

早晨血压飙升与糖尿病患者的自主神经病变和外周血管疾病有关。
尽管血管和自主神经系统参与了血压晨峰 (MBPS) 的调节,但关于糖尿病人群中 MBPS 临床相关性的数据很少,尤其是在糖尿病并发症方面。本研究旨在调查糖尿病中 MBPS 的预测因素和相关性。在一项包括 167 名糖尿病患者(年龄 58.5 ± 11.1 岁,病程 15.9 ± 12.1 岁)的横断面研究中,测量了临床变量、糖尿病和神经病理性并发症以及 MBPS(使用 24 小时动态血压监测)。MBPS 的上四分位数 (>30.5 mmHg) 与较高的腰围值 ( P = 0.027)、甘油三酯 ( P = 0.021) 和密歇根糖尿病神经病变评分 ( P = 0.042),HDL 胆固醇较低 ( P = 0.030),并且存在心血管自主神经病变 (CAN) ( P = 0.016) 和外周血管疾病 (PVD) ( P < 0.0001)。在逻辑回归分析中,PVD(优势比:10.2,P = 0.001)、CAN(优势比:6.09,P = 0.016)和舒张压(BP)(优势比:1.06,P = 0.022)预测 MBPS 上限四分位数 ( r 2 = 0.20, P = 0.0005)。在多元回归分析中,PVD ( P = 0.002) 和舒张压 ( P = 0.003) 是 MBPS ( r 2 = 0.20)。MBPS 上四分位数与血压下降相关(收缩压昼夜降低 > 10%)(P = 0.012),MBPS 与收缩压(rho = 0.41,P < 0.0001)和舒张压昼夜降低呈正相关。总之,代谢综合征的标志、舒张压、CAN 和 PVD 是糖尿病人群 MBPS 的主要预测因子。过度的 MBPS 和非浸渍不是同时发生的 24 小时血压变化。自主神经功能障碍可能会加剧 MBPS 现象。































 京公网安备 11010802027423号
京公网安备 11010802027423号