当前位置:
X-MOL 学术
›
JACC Cardiovasc. Inte.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Risk-Adjusting Key Outcome Measures in a Clinical Quality PCI Registry: Development of a Highly Predictive Model Without the Need to Exclude High-Risk Conditions.
JACC: Cardiovascular Interventions ( IF 11.7 ) Pub Date : 2019-10-07 , DOI: 10.1016/j.jcin.2019.07.002 Mark Tacey 1 , Diem T Dinh 2 , Nick Andrianopoulos 2 , Angela L Brennan 2 , Dion Stub 3 , Danny Liew 2 , Christopher M Reid 4 , Stephen J Duffy 3 , Jeffrey Lefkovits 5
JACC: Cardiovascular Interventions ( IF 11.7 ) Pub Date : 2019-10-07 , DOI: 10.1016/j.jcin.2019.07.002 Mark Tacey 1 , Diem T Dinh 2 , Nick Andrianopoulos 2 , Angela L Brennan 2 , Dion Stub 3 , Danny Liew 2 , Christopher M Reid 4 , Stephen J Duffy 3 , Jeffrey Lefkovits 5
Affiliation
|
OBJECTIVES
This study sought to determine the most risk-adjustment model for 30-day all-cause mortality in order to report risk-adjusted outcomes. The study also explored whether the exclusion of extreme high-risk conditions of cardiogenic shock, intubated out-of-hospital cardiac arrest (OHCA), or the need for mechanical ventricular support affected the model's predictive accuracy.
BACKGROUND
Robust risk-adjustment models are a critical component of clinical quality registries, allowing outcomes to be reported in a fair and meaningful way. The Victorian Cardiac Outcomes Registry encompasses all 30 hospitals in the state of Victoria, Australia, that undertake percutaneous coronary intervention.
METHODS
Data were collected on 27,544 consecutive percutaneous coronary intervention procedures from 2014 to 2016. Twenty-eight patient risk factors and procedural variables were considered in the modeling process. The multivariable logistic regression analysis considered derivation and validation datasets, along with a temporal validation period.
RESULTS
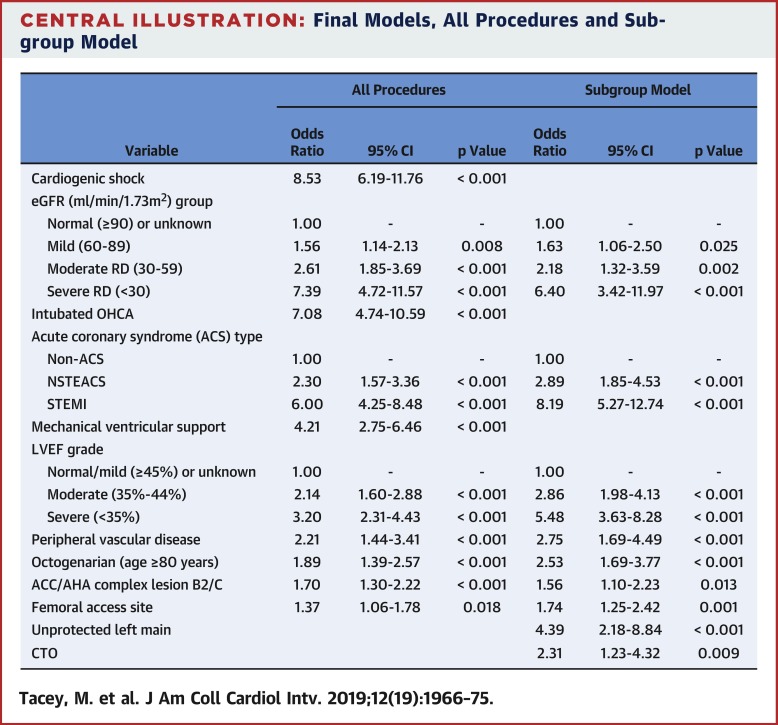
The model included risk-adjustment for cardiogenic shock, intubated OHCA, estimated glomerular filtration rate, left ventricular ejection fraction, angina type, mechanical ventricular support, ≥80 years of age, lesion complexity, percutaneous access site, and peripheral vascular disease. The C-statistic for the derivation dataset was 0.921 (95% confidence interval: 0.905 to 0.936), with C-statistics of 0.931 and 0.934 for 2 validation datasets reflecting the 2014 to 2016 and 2017 periods. Subgroup modeling excluding cardiogenic shock and intubated OHCA provided similar risk-adjusted outcomes (p = 0.32).
CONCLUSIONS
Our study has developed a highly predictive risk-adjustment model for 30-day mortality that included high-risk presentations. Therefore, we do not need to exclude high-risk cases in our model when determining risk-adjusted outcomes.
中文翻译:

临床质量PCI注册表中的风险调整关键成果指标:无需排除高风险条件就可以开发出高度预测的模型。
目的本研究旨在确定30天全因死亡率的最大风险调整模型,以报告风险调整后的结果。该研究还探讨了排除心源性休克的极高风险条件,气管插管的院外心脏骤停(OHCA)或对机械心室支持的需求是否会影响模型的预测准确性。背景技术稳健的风险调整模型是临床质量注册中心的重要组成部分,可以以公正,有意义的方式报告结果。维多利亚州心脏结局登记处包括澳大利亚维多利亚州的所有30家进行经皮冠状动脉介入治疗的医院。方法收集2014年至2016年连续进行的27,544例经皮冠状动脉介入治疗程序的数据。在建模过程中考虑了28个患者的危险因素和程序变量。多变量逻辑回归分析考虑了推导和验证数据集以及时间验证期。结果该模型包括心源性休克的风险调整,OHCA插管,估计的肾小球滤过率,左心室射血分数,心绞痛类型,机械性心室支持,≥80岁,病变复杂度,经皮穿刺部位和周围血管疾病。推导数据集的C统计量为0.921(95%置信区间:0.905至0.936),两个验证数据集的C统计量分别为0.931和0.934,反映了2014年至2016年和2017年的时间段。除心源性休克和插管式OHCA以外的亚组模型提供了相似的风险调整后结果(p = 0.32)。结论我们的研究为30天死亡率建立了高度预测的风险调整模型,其中包括高风险表现。因此,在确定风险调整后的结果时,我们无需在模型中排除高风险案例。
更新日期:2019-10-07
中文翻译:

临床质量PCI注册表中的风险调整关键成果指标:无需排除高风险条件就可以开发出高度预测的模型。
目的本研究旨在确定30天全因死亡率的最大风险调整模型,以报告风险调整后的结果。该研究还探讨了排除心源性休克的极高风险条件,气管插管的院外心脏骤停(OHCA)或对机械心室支持的需求是否会影响模型的预测准确性。背景技术稳健的风险调整模型是临床质量注册中心的重要组成部分,可以以公正,有意义的方式报告结果。维多利亚州心脏结局登记处包括澳大利亚维多利亚州的所有30家进行经皮冠状动脉介入治疗的医院。方法收集2014年至2016年连续进行的27,544例经皮冠状动脉介入治疗程序的数据。在建模过程中考虑了28个患者的危险因素和程序变量。多变量逻辑回归分析考虑了推导和验证数据集以及时间验证期。结果该模型包括心源性休克的风险调整,OHCA插管,估计的肾小球滤过率,左心室射血分数,心绞痛类型,机械性心室支持,≥80岁,病变复杂度,经皮穿刺部位和周围血管疾病。推导数据集的C统计量为0.921(95%置信区间:0.905至0.936),两个验证数据集的C统计量分别为0.931和0.934,反映了2014年至2016年和2017年的时间段。除心源性休克和插管式OHCA以外的亚组模型提供了相似的风险调整后结果(p = 0.32)。结论我们的研究为30天死亡率建立了高度预测的风险调整模型,其中包括高风险表现。因此,在确定风险调整后的结果时,我们无需在模型中排除高风险案例。







































 京公网安备 11010802027423号
京公网安备 11010802027423号