当前位置:
X-MOL 学术
›
Mucosal Immunol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Non-hematopoietic STAT6 induces epithelial tight junction dysfunction and promotes intestinal inflammation and tumorigenesis.
Mucosal Immunology ( IF 7.9 ) Pub Date : 2019-09-18 , DOI: 10.1038/s41385-019-0204-y Yuli Lin 1, 2 , Bingji Li 1 , Xuguang Yang 3, 4, 5 , Ting Liu 1 , Tiancong Shi 1 , Bo Deng 6 , Yubin Zhang 7 , Lijun Jia 3 , Zhengfan Jiang 8 , Rui He 1
Mucosal Immunology ( IF 7.9 ) Pub Date : 2019-09-18 , DOI: 10.1038/s41385-019-0204-y Yuli Lin 1, 2 , Bingji Li 1 , Xuguang Yang 3, 4, 5 , Ting Liu 1 , Tiancong Shi 1 , Bo Deng 6 , Yubin Zhang 7 , Lijun Jia 3 , Zhengfan Jiang 8 , Rui He 1
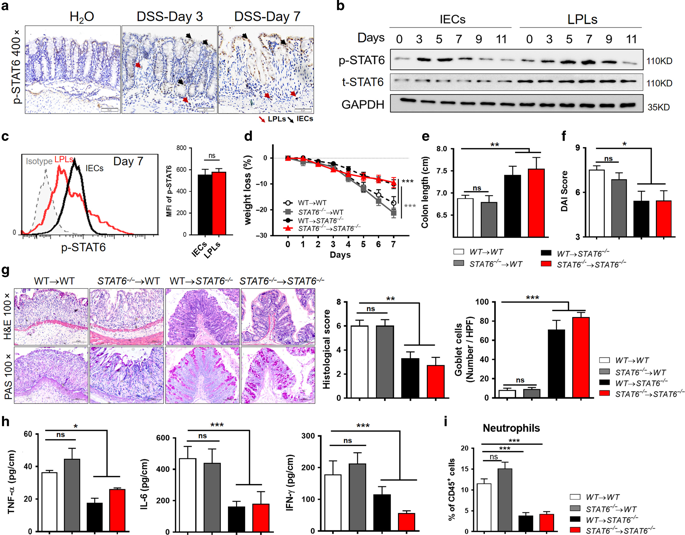
Affiliation
|
Enhanced gut permeability due to dysregulated epithelial tight junction is often associated with inflammatory bowel diseases (IBD), which have a greater risk for developing colorectal cancer. STAT6 activation was detected in inflamed colonic epithelium of active IBD patients, suggesting a role of epithelial STAT6 in colitis development. Here, we demonstrated that non-hematopoietic STAT6, but not hematopoietic STAT6, triggered DSS-induced colitis and subsequent tumorigenesis. This could be due to the enhancing-effect of STAT6 on gut permeability and microbiota translocation via interruption of epithelial tight junction integrity. Mechanistically, long-myosin light-chain kinase (MLCK1) was identified as a target of STAT6, leading to epithelial tight junction dysfunction and microbiota-driven colitis. Furthermore, neutralization of IL-13, which was primarily derived from type 2 innate lymphoid cells (ILC2) in a microbiota-dependent way, inhibited epithelial STAT6 activation and improved gut permeability and DSS-induced colitis. Importantly, pharmacological inhibition of STAT6 reduces murine intestinal tumor formation, and tumoral p-STAT6 levels positively correlated to the clinical stage and poor prognosis of human colorectal cancer. Thus, our study reveals a direct role of STAT6 in the disruption of epithelial tight junction integrity and colitis development, and suggests STAT6 as a potential therapeutic and prophylactic target for IBD and colitis-associated cancer.
中文翻译:

非造血 STAT6 诱导上皮紧密连接功能障碍并促进肠道炎症和肿瘤发生。
由于上皮紧密连接失调导致的肠道通透性增强通常与炎症性肠病 (IBD) 相关,而炎症性肠病具有更大的患结直肠癌的风险。在活动性 IBD 患者的发炎结肠上皮中检测到 STAT6 激活,表明上皮 STAT6 在结肠炎发展中的作用。在这里,我们证明了非造血 STAT6,而不是造血 STAT6,触发了 DSS 诱导的结肠炎和随后的肿瘤发生。这可能是由于 STAT6 通过中断上皮紧密连接完整性对肠道通透性和微生物群易位的增强作用。从机制上讲,长肌球蛋白轻链激酶 (MLCK1) 被确定为 STAT6 的靶标,导致上皮紧密连接功能障碍和微生物群驱动的结肠炎。此外,IL-13 的中和,它主要以微生物群依赖性方式来源于 2 型先天性淋巴样细胞 (ILC2),抑制上皮 STAT6 激活并改善肠道通透性和 DSS 诱导的结肠炎。重要的是,STAT6 的药理学抑制减少了小鼠肠道肿瘤的形成,并且肿瘤 p-STAT6 水平与人类结直肠癌的临床分期和不良预后呈正相关。因此,我们的研究揭示了 STAT6 在破坏上皮紧密连接完整性和结肠炎发展中的直接作用,并表明 STAT6 作为 IBD 和结肠炎相关癌症的潜在治疗和预防靶点。STAT6 的药理学抑制减少了小鼠肠道肿瘤的形成,肿瘤 p-STAT6 水平与人类结直肠癌的临床分期和不良预后呈正相关。因此,我们的研究揭示了 STAT6 在破坏上皮紧密连接完整性和结肠炎发展中的直接作用,并表明 STAT6 作为 IBD 和结肠炎相关癌症的潜在治疗和预防靶点。STAT6 的药理学抑制减少了小鼠肠道肿瘤的形成,肿瘤 p-STAT6 水平与人类结直肠癌的临床分期和不良预后呈正相关。因此,我们的研究揭示了 STAT6 在破坏上皮紧密连接完整性和结肠炎发展中的直接作用,并表明 STAT6 作为 IBD 和结肠炎相关癌症的潜在治疗和预防靶点。
更新日期:2019-09-19
中文翻译:

非造血 STAT6 诱导上皮紧密连接功能障碍并促进肠道炎症和肿瘤发生。
由于上皮紧密连接失调导致的肠道通透性增强通常与炎症性肠病 (IBD) 相关,而炎症性肠病具有更大的患结直肠癌的风险。在活动性 IBD 患者的发炎结肠上皮中检测到 STAT6 激活,表明上皮 STAT6 在结肠炎发展中的作用。在这里,我们证明了非造血 STAT6,而不是造血 STAT6,触发了 DSS 诱导的结肠炎和随后的肿瘤发生。这可能是由于 STAT6 通过中断上皮紧密连接完整性对肠道通透性和微生物群易位的增强作用。从机制上讲,长肌球蛋白轻链激酶 (MLCK1) 被确定为 STAT6 的靶标,导致上皮紧密连接功能障碍和微生物群驱动的结肠炎。此外,IL-13 的中和,它主要以微生物群依赖性方式来源于 2 型先天性淋巴样细胞 (ILC2),抑制上皮 STAT6 激活并改善肠道通透性和 DSS 诱导的结肠炎。重要的是,STAT6 的药理学抑制减少了小鼠肠道肿瘤的形成,并且肿瘤 p-STAT6 水平与人类结直肠癌的临床分期和不良预后呈正相关。因此,我们的研究揭示了 STAT6 在破坏上皮紧密连接完整性和结肠炎发展中的直接作用,并表明 STAT6 作为 IBD 和结肠炎相关癌症的潜在治疗和预防靶点。STAT6 的药理学抑制减少了小鼠肠道肿瘤的形成,肿瘤 p-STAT6 水平与人类结直肠癌的临床分期和不良预后呈正相关。因此,我们的研究揭示了 STAT6 在破坏上皮紧密连接完整性和结肠炎发展中的直接作用,并表明 STAT6 作为 IBD 和结肠炎相关癌症的潜在治疗和预防靶点。STAT6 的药理学抑制减少了小鼠肠道肿瘤的形成,肿瘤 p-STAT6 水平与人类结直肠癌的临床分期和不良预后呈正相关。因此,我们的研究揭示了 STAT6 在破坏上皮紧密连接完整性和结肠炎发展中的直接作用,并表明 STAT6 作为 IBD 和结肠炎相关癌症的潜在治疗和预防靶点。





















































 京公网安备 11010802027423号
京公网安备 11010802027423号