当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Impact of LDL Cholesterol on Microvascular Versus Macrovascular Disease
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2019-09-01 , DOI: 10.1016/j.jacc.2019.07.037
Frida Emanuelsson 1 , Børge G Nordestgaard 2 , Anne Tybjærg-Hansen 3 , Marianne Benn 1
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2019-09-01 , DOI: 10.1016/j.jacc.2019.07.037
Frida Emanuelsson 1 , Børge G Nordestgaard 2 , Anne Tybjærg-Hansen 3 , Marianne Benn 1
Affiliation
|
BACKGROUND
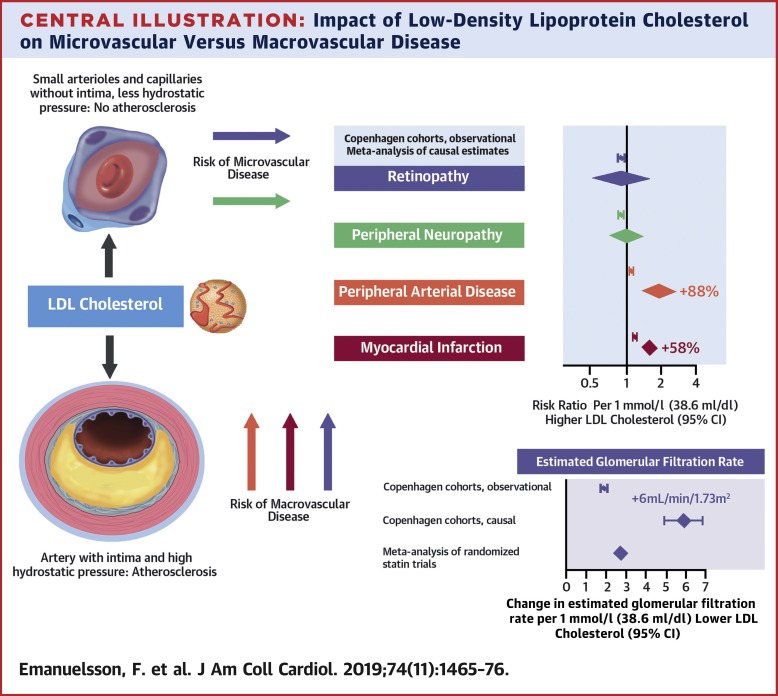
Low-density lipoprotein cholesterol (LDL-C) is causally associated with a high risk of coronary artery disease. Whether this also holds for a spectrum of peripheral vascular diseases is unknown. OBJECTIVES
The purpose of this study was to determine whether high LDL-C causally relates to risk of retinopathy, neuropathy, chronic kidney disease (CKD), and peripheral arterial disease (PAD) in the general population. METHODS
One-sample Mendelian randomization (MR) of 116,419 Danish individuals, 2-sample MR on summary-level data from the Global Lipid Genetics Consortium (GLGC) (n = 94,595) and the UK Biobank (n = 408,455), and meta-analysis of randomized statin trials (n = 64,134) were performed. RESULTS
Observationally, high LDL-C did not associate with high risk of retinopathy or neuropathy. There were stepwise increases in risk of CKD and PAD with higher LDL-C (both p for trend <0.001), with hazard ratios of 1.05 (95% confidence interval [CI]: 0.97 to 1.13) for CKD, and 1.41 (95% CI: 1.23 to 1.62) for PAD in individuals with LDL-C above the 95th percentile versus below the 50th percentile. In genetic, causal analyses in the Copenhagen studies, the risk ratio of disease for a 1 mmol/l higher LDL-C was 1.06 (95% CI: 0.24 to 4.58) for retinopathy, 1.05 (95% CI: 0.64 to 1.72) for neuropathy, 3.83 (95% CI: 2.00 to 7.34) for CKD, and 2.09 (95% CI: 1.30 to 2.38) for PAD. Summary-level data from the GLGC and the UK Biobank for retinopathy, neuropathy, and PAD gave similar results. For CKD, a 1-mmol/l lower LDL-C conferred a higher eGFR of 1.95 ml/min/1.73 m2 (95% CI: 1.88 to 2.02 ml/min/1.73 m2) observationally, 5.92 ml/min/1.73 m2 (95% CI: 4.97 to 6.86 ml/min/1.73 m2) genetically, and 2.69 ml/min/1.73 m2 (95% CI: 1.48 to 3.94 ml/min/1.73 m2) through statin therapy. CONCLUSIONS
High LDL-C was not causally associated with risk of retinopathy and neuropathy; however, high LDL-C was observationally and genetically associated with high risks of PAD and CKD, suggesting that LDL-C is causally involved in the pathogenesis of these diseases.
中文翻译:

低密度脂蛋白胆固醇对微血管与大血管疾病的影响
背景低密度脂蛋白胆固醇(LDL-C)与冠状动脉疾病的高风险有因果关系。这是否也适用于一系列外周血管疾病尚不清楚。目的 本研究的目的是确定高 LDL-C 是否与一般人群中视网膜病变、神经病变、慢性肾病 (CKD) 和外周动脉疾病 (PAD) 的风险存在因果关系。方法 116,419 名丹麦人的单样本孟德尔随机化 (MR),来自全球脂质遗传学联盟 (GLGC) (n = 94,595) 和英国生物银行 (n = 408,455) 的汇总级数据的 2 样本 MR,以及元对随机他汀类试验(n = 64,134)进行了分析。结果 从观察上看,高 LDL-C 与视网膜病变或神经病变的高风险无关。CKD 和 PAD 的风险随着 LDL-C 的升高而逐步增加(趋势均为 p<0.001),CKD 的风险比为 1.05(95% 置信区间 [CI]:0.97 至 1.13)和 1.41(95% CI:1.23 至 1.62)对于 LDL-C 高于 95% 与低于 50% 的个体的 PAD。在哥本哈根研究的遗传、因果分析中,LDL-C 升高 1 mmol/l 的疾病风险比对于视网膜病变为 1.06(95% CI:0.24 至 4.58),对于视网膜病变为 1.05(95% CI:0.64 至 1.72)神经病变,CKD 为 3.83(95% CI:2.00 至 7.34),PAD 为 2.09(95% CI:1.30 至 2.38)。来自 GLGC 和英国生物银行的视网膜病变、神经病变和 PAD 的汇总数据给出了类似的结果。对于 CKD,低 1 mmol/l 的 LDL-C 赋予更高的 eGFR,为 1.95 ml/min/1.73 m2(95% CI:1.88 至 2.02 ml/min/1.73 m2),5.92 ml/min/1。73 平方米(95% CI:4.97 至 6.86 毫升/分钟/1.73 平方米)遗传,2.69 毫升/分钟/1.73 平方米(95% CI:1.48 至 3.94 毫升/分钟/1.73 平方米)通过他汀类药物治疗。结论 高 LDL-C 与视网膜病变和神经病变的风险没有因果关系;然而,高 LDL-C 在观察和遗传上与 PAD 和 CKD 的高风险相关,表明 LDL-C 与这些疾病的发病机制有关。
更新日期:2019-09-01
中文翻译:

低密度脂蛋白胆固醇对微血管与大血管疾病的影响
背景低密度脂蛋白胆固醇(LDL-C)与冠状动脉疾病的高风险有因果关系。这是否也适用于一系列外周血管疾病尚不清楚。目的 本研究的目的是确定高 LDL-C 是否与一般人群中视网膜病变、神经病变、慢性肾病 (CKD) 和外周动脉疾病 (PAD) 的风险存在因果关系。方法 116,419 名丹麦人的单样本孟德尔随机化 (MR),来自全球脂质遗传学联盟 (GLGC) (n = 94,595) 和英国生物银行 (n = 408,455) 的汇总级数据的 2 样本 MR,以及元对随机他汀类试验(n = 64,134)进行了分析。结果 从观察上看,高 LDL-C 与视网膜病变或神经病变的高风险无关。CKD 和 PAD 的风险随着 LDL-C 的升高而逐步增加(趋势均为 p<0.001),CKD 的风险比为 1.05(95% 置信区间 [CI]:0.97 至 1.13)和 1.41(95% CI:1.23 至 1.62)对于 LDL-C 高于 95% 与低于 50% 的个体的 PAD。在哥本哈根研究的遗传、因果分析中,LDL-C 升高 1 mmol/l 的疾病风险比对于视网膜病变为 1.06(95% CI:0.24 至 4.58),对于视网膜病变为 1.05(95% CI:0.64 至 1.72)神经病变,CKD 为 3.83(95% CI:2.00 至 7.34),PAD 为 2.09(95% CI:1.30 至 2.38)。来自 GLGC 和英国生物银行的视网膜病变、神经病变和 PAD 的汇总数据给出了类似的结果。对于 CKD,低 1 mmol/l 的 LDL-C 赋予更高的 eGFR,为 1.95 ml/min/1.73 m2(95% CI:1.88 至 2.02 ml/min/1.73 m2),5.92 ml/min/1。73 平方米(95% CI:4.97 至 6.86 毫升/分钟/1.73 平方米)遗传,2.69 毫升/分钟/1.73 平方米(95% CI:1.48 至 3.94 毫升/分钟/1.73 平方米)通过他汀类药物治疗。结论 高 LDL-C 与视网膜病变和神经病变的风险没有因果关系;然而,高 LDL-C 在观察和遗传上与 PAD 和 CKD 的高风险相关,表明 LDL-C 与这些疾病的发病机制有关。

































 京公网安备 11010802027423号
京公网安备 11010802027423号