Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Dracorhodin perchlorate protects pancreatic β-cells against glucotoxicity- or lipotoxicity-induced dysfunction and apoptosis in vitro and in vivo.
The FEBS Journal ( IF 5.5 ) Pub Date : 2019-08-14 , DOI: 10.1111/febs.15020 Lei Liu 1 , Chen Liang 2 , Pucheng Mei 2 , Hong Zhu 2 , Meiling Hou 1 , Chunlei Yu 1 , Zhenbo Song 2 , Yongli Bao 2 , Yanxin Huang 2 , Jingwen Yi 1 , Shuyue Wang 2 , Yin Wu 2 , Lihua Zheng 2 , Ying Sun 1 , Guannan Wang 2 , Mingxin Huo 3 , Shaonian Yang 2, 4 , Luguo Sun 2 , Yuxin Li 1
The FEBS Journal ( IF 5.5 ) Pub Date : 2019-08-14 , DOI: 10.1111/febs.15020 Lei Liu 1 , Chen Liang 2 , Pucheng Mei 2 , Hong Zhu 2 , Meiling Hou 1 , Chunlei Yu 1 , Zhenbo Song 2 , Yongli Bao 2 , Yanxin Huang 2 , Jingwen Yi 1 , Shuyue Wang 2 , Yin Wu 2 , Lihua Zheng 2 , Ying Sun 1 , Guannan Wang 2 , Mingxin Huo 3 , Shaonian Yang 2, 4 , Luguo Sun 2 , Yuxin Li 1
Affiliation
|
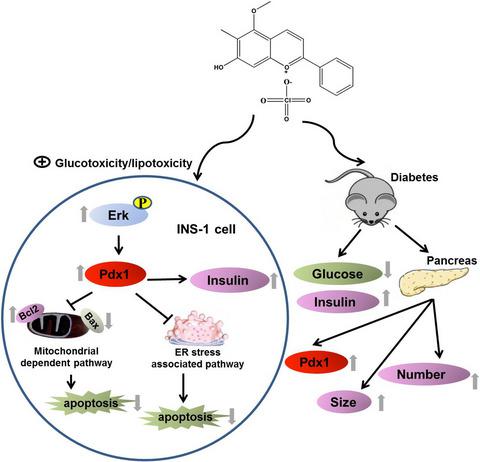
Glucotoxicity or lipotoxicity leads to hyperglycemia and insulin secretion deficiency, which are important causes for the onset of type 2 diabetes mellitus (T2DM). Thus, the restoration of β-cell function is a long-sought goal in diabetes research. Previous studies have implicated pancreatic and duodenal homeobox 1 gene (Pdx1) in β-cell function and insulin secretion. In this study, we established a Pdx1 promoter-dependent luciferase system and identified the natural compound dracorhodin perchlorate (DP) as an effective promotor of Pdx1 expression. We further demonstrated that DP could significantly inhibit β-cell apoptosis induced by 33 mm glucose or 200 μm palmitate by interfering with endoplasmic reticulum stress and mitochondrial pathways and enhance insulin secretion as well. These effects were associated with enhanced activities of Erk1/2, which in turn promoted Pdx1 expression and increased the ratio of Bcl2/Bax, since inhibition of the Erk1/2 pathway abolished the DP-induced expression of Pdx1 and suppression of apoptosis. In addition, our in vivo results in diabetic mice indicated that DP treatment lowered blood glucose, raised insulin levels, enhanced Pdx1 expression and increased islet size and number in the pancreas of diabetic mice. Our findings suggest that Pdx1 is a potential target molecule of DP in the treatment of T2DM via the inhibition of glucotoxicity- or lipotoxicity- induced β-cell apoptosis and the attenuation of insulin secretion dysfunction.
中文翻译:

Dracorhodin高氯酸盐在体外和体内保护胰腺β细胞免受糖毒性或脂毒性诱导的功能障碍和细胞凋亡。
糖毒性或脂毒性会导致高血糖症和胰岛素分泌不足,这是2型糖尿病(T2DM)发作的重要原因。因此,β细胞功能的恢复是糖尿病研究的长期目标。先前的研究涉及胰腺和十二指肠同源异型盒1基因(Pdx1)的β细胞功能和胰岛素分泌。在这项研究中,我们建立了一个依赖Pdx1启动子的荧光素酶系统,并确定了天然化合物高氯龙素(DP)是Pdx1表达的有效促进剂。我们进一步证明,DP可以通过干扰内质网应激和线粒体途径并增强胰岛素分泌来显着抑制33 mm葡萄糖或200μm棕榈酸酯诱导的β细胞凋亡。这些影响与Erk1 / 2的活性增强有关,由于抑制Erk1 / 2途径消除了DP诱导的Pdx1表达并抑制了细胞凋亡,因此反过来又促进了Pdx1的表达并增加了Bcl2 / Bax的比率。另外,我们在糖尿病小鼠中的体内结果表明,DP治疗降低了糖尿病小鼠的血糖,提高了胰岛素水平,增强了Pdx1表达并增加了胰岛的大小和数量。我们的发现表明,Pdx1通过抑制糖毒性或脂毒性诱导的β细胞凋亡和减轻胰岛素分泌功能障碍,是治疗T2DM中DP的潜在靶分子。我们在糖尿病小鼠中的体内结果表明,DP治疗可降低糖尿病小鼠的血糖,提高胰岛素水平,增强Pdx1表达并增加胰岛的大小和数量。我们的发现表明,Pdx1通过抑制糖毒性或脂毒性诱导的β细胞凋亡和减轻胰岛素分泌功能障碍,是治疗T2DM中DP的潜在靶分子。我们在糖尿病小鼠中的体内结果表明,DP治疗可降低糖尿病小鼠的血糖,提高胰岛素水平,增强Pdx1表达并增加胰岛的大小和数量。我们的发现表明,Pdx1通过抑制糖毒性或脂毒性诱导的β细胞凋亡和减轻胰岛素分泌功能障碍,是治疗T2DM中DP的潜在靶分子。
更新日期:2019-08-14
中文翻译:

Dracorhodin高氯酸盐在体外和体内保护胰腺β细胞免受糖毒性或脂毒性诱导的功能障碍和细胞凋亡。
糖毒性或脂毒性会导致高血糖症和胰岛素分泌不足,这是2型糖尿病(T2DM)发作的重要原因。因此,β细胞功能的恢复是糖尿病研究的长期目标。先前的研究涉及胰腺和十二指肠同源异型盒1基因(Pdx1)的β细胞功能和胰岛素分泌。在这项研究中,我们建立了一个依赖Pdx1启动子的荧光素酶系统,并确定了天然化合物高氯龙素(DP)是Pdx1表达的有效促进剂。我们进一步证明,DP可以通过干扰内质网应激和线粒体途径并增强胰岛素分泌来显着抑制33 mm葡萄糖或200μm棕榈酸酯诱导的β细胞凋亡。这些影响与Erk1 / 2的活性增强有关,由于抑制Erk1 / 2途径消除了DP诱导的Pdx1表达并抑制了细胞凋亡,因此反过来又促进了Pdx1的表达并增加了Bcl2 / Bax的比率。另外,我们在糖尿病小鼠中的体内结果表明,DP治疗降低了糖尿病小鼠的血糖,提高了胰岛素水平,增强了Pdx1表达并增加了胰岛的大小和数量。我们的发现表明,Pdx1通过抑制糖毒性或脂毒性诱导的β细胞凋亡和减轻胰岛素分泌功能障碍,是治疗T2DM中DP的潜在靶分子。我们在糖尿病小鼠中的体内结果表明,DP治疗可降低糖尿病小鼠的血糖,提高胰岛素水平,增强Pdx1表达并增加胰岛的大小和数量。我们的发现表明,Pdx1通过抑制糖毒性或脂毒性诱导的β细胞凋亡和减轻胰岛素分泌功能障碍,是治疗T2DM中DP的潜在靶分子。我们在糖尿病小鼠中的体内结果表明,DP治疗可降低糖尿病小鼠的血糖,提高胰岛素水平,增强Pdx1表达并增加胰岛的大小和数量。我们的发现表明,Pdx1通过抑制糖毒性或脂毒性诱导的β细胞凋亡和减轻胰岛素分泌功能障碍,是治疗T2DM中DP的潜在靶分子。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号