JAMA Neurology ( IF 20.4 ) Pub Date : 2019-12-01 , DOI: 10.1001/jamaneurol.2019.2531 Yuesong Pan 1, 2, 3, 4 , Jordan J Elm 5 , Hao Li 1, 2, 3, 4 , J Donald Easton 6 , Yilong Wang 1, 2, 3, 4 , Mary Farrant 6 , Xia Meng 1, 2, 3, 4 , Anthony S Kim 6 , Xingquan Zhao 1, 2, 3, 4 , William J Meurer 7, 8 , Liping Liu 1, 2, 3, 4 , Dennis Dietrich 9 , Yongjun Wang 1, 2, 3, 4 , S Claiborne Johnston 10
|
Importance Dual antiplatelet therapy with clopidogrel and aspirin is effective for secondary prevention after minor ischemic stroke or transient ischemic attack (TIA). Uncertainties remained about the optimal duration of dual antiplatelet therapy for minor stroke or TIA.
Objective To obtain precise estimates of efficacy and risk of dual antiplatelet therapy after minor ischemic stroke or TIA.
Design, Setting, and Participants This analysis pooled individual patient–level data from 2 large-scale randomized clinical trials that evaluated clopidogrel-aspirin as a treatment to prevent stroke after a minor stroke or high-risk TIA. The Clopidogrel in High-Risk Patients With Acute Non-Disabling Cerebrovascular Events (CHANCE) trial enrolled patients at 114 sites in China from October 1, 2009, to July 30, 2012. The Platelet-Oriented Inhibition in New TIA and Minor Ischemic Stroke (POINT) trial enrolled patients at 269 international sites from May 28, 2010, to December 19, 2017. Both were followed up for 90 days. Data analysis occurred from November 2018 to May 2019.
Interventions In the 2 trials, patients with minor stroke or high-risk TIA were randomized to clopidogrel-aspirin or aspirin alone within 12 hours (POINT) or 24 hours (CHANCE) of symptom onset.
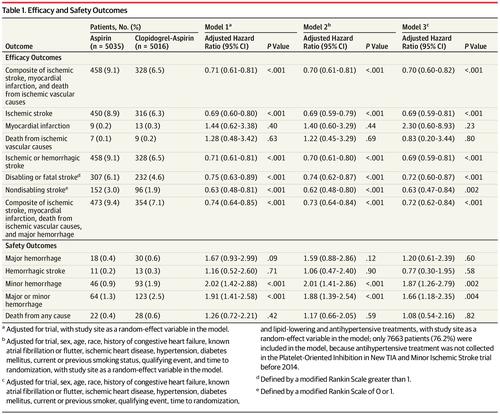
Main Outcomes and Measures The primary efficacy outcome was a major ischemic event (ischemic stroke, myocardial infarction, or death from ischemic vascular causes). The primary safety outcome was major hemorrhage.
Results The study enrolled 5170 patients (CHANCE) and 4881 patients (POINT). Analysis included individual data from 10 051 patients (5016 in the clopidogrel-aspirin treatment group and 5035 in the control group) with a median age of 63.2 (interquartile range, 55.0-72.9) years; 6106 patients (60.8%) were male. Clopidogrel-aspirin treatment reduced the risk of major ischemic events at 90 days compared with aspirin alone (328 of 5016 [6.5%] vs 458 of 5035 [9.1%]; hazard ratio [HR], 0.70 [95% CI, 0.61-0.81]; P < .001), mainly within the first 21 days (263 of 5016 [5.2%] vs 391 of 5035 [7.8%]; HR, 0.66 [95% CI, 0.56-0.77]; P < .001), but not from day 22 to day 90. No evidence of heterogeneity of treatment outcome across trials or prespecified subgroups was observed. Major hemorrhages were more frequent in the clopidogrel-aspirin group, but the difference was nonsignificant.
Conclusions and Relevance In this analysis of the POINT and CHANCE trials, the benefit of dual antiplatelet therapy appeared to be confined to the first 21 days after minor ischemic stroke or high-risk TIA.



























 京公网安备 11010802027423号
京公网安备 11010802027423号