当前位置:
X-MOL 学术
›
Prostate Cancer Prostatic. Dis.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Preoperative PI-RADS Version 2 scores helps improve accuracy of clinical nomograms for predicting pelvic lymph node metastasis at radical prostatectomy.
Prostate Cancer and Prostatic Diseases ( IF 5.1 ) Pub Date : 2019-08-05 , DOI: 10.1038/s41391-019-0164-z Cong Huang 1, 2 , Gang Song 1, 2 , Huihui Wang 3 , Zhiyong Lin 3 , He Wang 3 , Guangjie Ji 1, 2 , Shouyi Zhang 4 , Yuanshan Guo 5 , Jie Li 6 , Zhengqing Bao 1, 2 , Peng Hong 1, 2 , Yicong Du 1, 2 , Peng Li 7 , Qun He 1, 2 , Shiming He 1, 2 , Yanqing Gong 1, 2 , Xiaoying Wang 3 , Liqun Zhou 1, 2
Prostate Cancer and Prostatic Diseases ( IF 5.1 ) Pub Date : 2019-08-05 , DOI: 10.1038/s41391-019-0164-z Cong Huang 1, 2 , Gang Song 1, 2 , Huihui Wang 3 , Zhiyong Lin 3 , He Wang 3 , Guangjie Ji 1, 2 , Shouyi Zhang 4 , Yuanshan Guo 5 , Jie Li 6 , Zhengqing Bao 1, 2 , Peng Hong 1, 2 , Yicong Du 1, 2 , Peng Li 7 , Qun He 1, 2 , Shiming He 1, 2 , Yanqing Gong 1, 2 , Xiaoying Wang 3 , Liqun Zhou 1, 2
Affiliation
|
BACKGROUND
Lymph node invasion (LNI) is a strong adverse prognostic factor in prostate cancer (PCa). The purpose of this study was to evaluate the role of Prostate Imaging Reporting and Data System version 2 (PI-RADSv2) scores for estimating the risk of LN metastasis. The study also aimed to investigate the additional value of PI-RADSv2 scores when used in combination with clinical nomograms for the prediction of LNI in patients with PCa.
METHODS
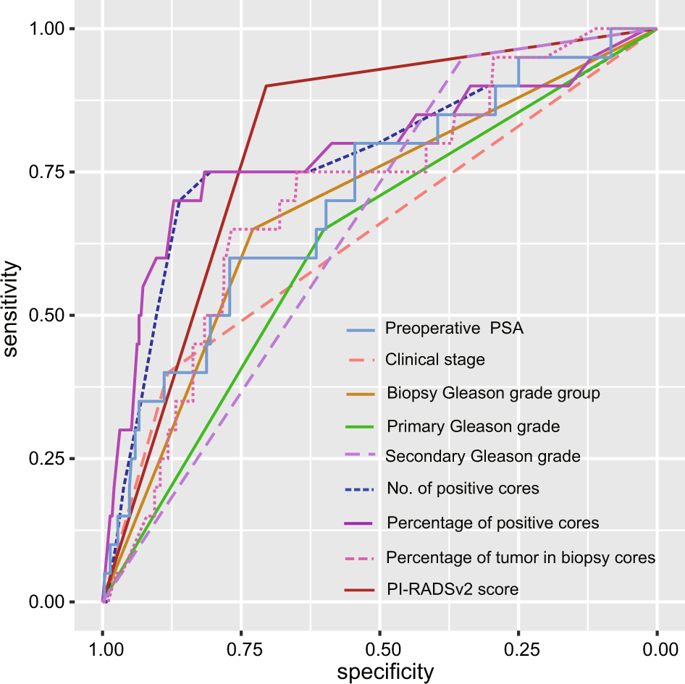
We retrospectively identified 308 patients who underwent multiparametric magnetic resonance imaging (mpMRI) and RP with pelvic lymph node dissection (PLND). Clinicopathological parameters and PI-RADSv2 scores were assessed. Univariate and multivariate logistic analyses were performed. The area under the receiver operating characteristic curves (AUCs) and decision curve analysis (DCA) were generated for assessing the incremental value of PI-RADSv2 scores combined with the Briganti and Memorial Sloan Kettering Cancer Center (MSKCC) nomograms.
RESULTS
Overall, 20 (6.5%) patients had LNI. At univariate analysis, all clinicopathological characteristics and PI-RADSv2 scores were significantly associated to LNI (p < 0.04). However, multivariate analysis revealed that only PI-RADSv2 scores and percentage of positive cores were independently significant (p ≤ 0.006). The PI-RADSv2 score was the most accurate predictor (AUC, 80.2%). The threshold of PI-RADSv2 score was 5, which provided high sensitivity (18/20, 90.0%) and negative predictive value (203/205, 99.0%). When PI-RADSv2 scores were combined with Briganti and MSKCC nomograms, the AUC value increased from 75.1 to 86.3% and from 79.2 to 87.9%, respectively (p ≤ 0.001). The DCA also demonstrated that the two nomograms plus PI-RADSv2 scores improved clinical risk prediction of LNI.
CONCLUSIONS
The patients with a PI-RADSv2 score <5 were associated with a very low risk of LNI in PCa. Preoperative PI-RADSv2 scores could help improve the accuracy of clinical nomograms for predicting pelvic LN metastasis at radical prostatectomy.
中文翻译:

术前 PI-RADS 第 2 版评分有助于提高临床列线图预测根治性前列腺切除术中盆腔淋巴结转移的准确性。
背景淋巴结浸润 (LNI) 是前列腺癌 (PCa) 的一个强烈的不良预后因素。本研究的目的是评估前列腺影像报告和数据系统第 2 版 (PI-RADSv2) 评分在估计 LN 转移风险方面的作用。该研究还旨在调查 PI-RADSv2 评分与临床列线图结合用于预测 PCa 患者 LNI 的附加价值。方法 我们回顾性地确定了 308 名接受多参数磁共振成像 (mpMRI) 和盆腔淋巴结清扫术 (PLND) RP 的患者。评估了临床病理参数和 PI-RADSv2 评分。进行了单变量和多变量逻辑分析。生成接受者操作特征曲线 (AUC) 和决策曲线分析 (DCA) 下的面积,以评估 PI-RADSv2 评分与 Briganti 和纪念斯隆凯特琳癌症中心 (MSKCC) 列线图相结合的增量值。结果 总体而言,20 名 (6.5%) 患者患有 LNI。在单变量分析中,所有临床病理特征和 PI-RADSv2 评分均与 LNI 显着相关(p < 0.04)。然而,多变量分析显示只有 PI-RADSv2 分数和阳性核心百分比是独立显着的(p ≤ 0.006)。PI-RADSv2 评分是最准确的预测指标(AUC,80.2%)。PI-RADSv2 评分的阈值为 5,提供了高灵敏度 (18/20, 90.0%) 和阴性预测值 (203/205, 99.0%)。当 PI-RADSv2 分数与 Briganti 和 MSKCC 列线图相结合时,AUC 值分别从 75.1% 增加到 86.3% 和从 79.2% 增加到 87.9% (p ≤ 0.001)。DCA 还证明,两个列线图加上 PI-RADSv2 评分提高了 LNI 的临床风险预测。结论 PI-RADSv2 评分 <5 的患者与 PCa 中极低的 LNI 风险相关。术前 PI-RADSv2 评分有助于提高临床列线图预测根治性前列腺切除术中盆腔淋巴结转移的准确性。
更新日期:2019-08-05
中文翻译:

术前 PI-RADS 第 2 版评分有助于提高临床列线图预测根治性前列腺切除术中盆腔淋巴结转移的准确性。
背景淋巴结浸润 (LNI) 是前列腺癌 (PCa) 的一个强烈的不良预后因素。本研究的目的是评估前列腺影像报告和数据系统第 2 版 (PI-RADSv2) 评分在估计 LN 转移风险方面的作用。该研究还旨在调查 PI-RADSv2 评分与临床列线图结合用于预测 PCa 患者 LNI 的附加价值。方法 我们回顾性地确定了 308 名接受多参数磁共振成像 (mpMRI) 和盆腔淋巴结清扫术 (PLND) RP 的患者。评估了临床病理参数和 PI-RADSv2 评分。进行了单变量和多变量逻辑分析。生成接受者操作特征曲线 (AUC) 和决策曲线分析 (DCA) 下的面积,以评估 PI-RADSv2 评分与 Briganti 和纪念斯隆凯特琳癌症中心 (MSKCC) 列线图相结合的增量值。结果 总体而言,20 名 (6.5%) 患者患有 LNI。在单变量分析中,所有临床病理特征和 PI-RADSv2 评分均与 LNI 显着相关(p < 0.04)。然而,多变量分析显示只有 PI-RADSv2 分数和阳性核心百分比是独立显着的(p ≤ 0.006)。PI-RADSv2 评分是最准确的预测指标(AUC,80.2%)。PI-RADSv2 评分的阈值为 5,提供了高灵敏度 (18/20, 90.0%) 和阴性预测值 (203/205, 99.0%)。当 PI-RADSv2 分数与 Briganti 和 MSKCC 列线图相结合时,AUC 值分别从 75.1% 增加到 86.3% 和从 79.2% 增加到 87.9% (p ≤ 0.001)。DCA 还证明,两个列线图加上 PI-RADSv2 评分提高了 LNI 的临床风险预测。结论 PI-RADSv2 评分 <5 的患者与 PCa 中极低的 LNI 风险相关。术前 PI-RADSv2 评分有助于提高临床列线图预测根治性前列腺切除术中盆腔淋巴结转移的准确性。































 京公网安备 11010802027423号
京公网安备 11010802027423号