当前位置:
X-MOL 学术
›
PLOS Pathog.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
MyD88 and IL-1R signaling drive antibacterial immunity and osteoclast-driven bone loss during Staphylococcus aureus osteomyelitis.
PLoS Pathogens ( IF 5.5 ) Pub Date : 2019-04-12 , DOI: 10.1371/journal.ppat.1007744
Nicole E Putnam 1 , Laura E Fulbright 2 , Jacob M Curry 2 , Caleb A Ford 3 , Jenna R Petronglo 1 , Andrew S Hendrix 2 , James E Cassat 1, 2, 3, 4, 5
PLoS Pathogens ( IF 5.5 ) Pub Date : 2019-04-12 , DOI: 10.1371/journal.ppat.1007744
Nicole E Putnam 1 , Laura E Fulbright 2 , Jacob M Curry 2 , Caleb A Ford 3 , Jenna R Petronglo 1 , Andrew S Hendrix 2 , James E Cassat 1, 2, 3, 4, 5
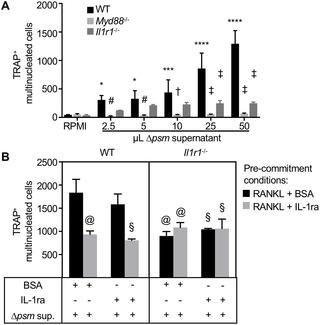
Affiliation
|
Staphylococcus aureus is able to infect virtually all organ systems and is a frequently isolated etiologic agent of osteomyelitis, a common and debilitating invasive infection of bone. Treatment of osteomyelitis requires invasive surgical procedures and prolonged antibiotic therapy, yet is frequently unsuccessful due to extensive pathogen-induced bone damage that can limit antibiotic penetration and immune cell influx to the infectious focus. We previously established that S. aureus triggers profound alterations in bone remodeling in a murine model of osteomyelitis, in part through the production of osteolytic toxins. However, staphylococcal strains lacking osteolytic toxins still incite significant bone destruction, suggesting that host immune responses are also major drivers of pathologic bone remodeling during osteomyelitis. The objective of this study was to identify host immune pathways that contribute to antibacterial immunity during S. aureus osteomyelitis, and to define how these immune responses alter bone homeostasis and contribute to bone destruction. We specifically focused on the interleukin-1 receptor (IL-1R) and downstream adapter protein MyD88 given the prominent role of this signaling pathway in both antibacterial immunity and osteo-immunologic crosstalk. We discovered that while IL-1R signaling is necessary for local control of bacterial replication during osteomyelitis, it also contributes to bone loss during infection. Mechanistically, we demonstrate that S. aureus enhances osteoclastogenesis of myeloid precursors in vitro, and increases the abundance of osteoclasts residing on bone surfaces in vivo. This enhanced osteoclast abundance translates to trabecular bone loss, and is dependent on intact IL-1R signaling. Collectively, these data define IL-1R signaling as a critical component of the host response to S. aureus osteomyelitis, but also demonstrate that IL-1R-dependent immune responses trigger collateral bone damage through activation of osteoclast-mediated bone resorption.
中文翻译:

在金黄色葡萄球菌骨髓炎期间,MyD88 和 IL-1R 信号驱动抗菌免疫和破骨细胞驱动的骨质流失。
金黄色葡萄球菌几乎能够感染所有器官系统,并且是骨髓炎(一种常见且使人衰弱的骨侵袭性感染)的常见分离病原体。骨髓炎的治疗需要侵入性外科手术和长期抗生素治疗,但由于病原体引起的广泛骨损伤会限制抗生素渗透和免疫细胞流入感染灶,因此治疗常常不成功。我们之前确定,金黄色葡萄球菌在小鼠骨髓炎模型中引发骨重塑的深刻改变,部分是通过产生溶骨毒素来实现的。然而,缺乏溶骨毒素的葡萄球菌菌株仍然会引起显着的骨质破坏,这表明宿主免疫反应也是骨髓炎期间病理性骨重塑的主要驱动因素。本研究的目的是确定金黄色葡萄球菌骨髓炎期间有助于抗菌免疫的宿主免疫途径,并确定这些免疫反应如何改变骨稳态并导致骨破坏。鉴于该信号通路在抗菌免疫和骨免疫串扰中的突出作用,我们特别关注白细胞介素 1 受体 (IL-1R) 和下游接头蛋白 MyD88。我们发现,虽然 IL-1R 信号传导对于骨髓炎期间细菌复制的局部控制是必要的,但它也会导致感染期间的骨质流失。从机制上讲,我们证明金黄色葡萄球菌在体外增强骨髓前体的破骨细胞生成,并在体内增加驻留在骨表面的破骨细胞的丰度。这种增强的破骨细胞丰度会导致小梁骨丢失,并且依赖于完整的 IL-1R 信号传导。 总的来说,这些数据将 IL-1R 信号传导定义为宿主对金黄色葡萄球菌骨髓炎反应的关键组成部分,但也证明 IL-1R 依赖性免疫反应通过激活破骨细胞介导的骨吸收触发附带骨损伤。
更新日期:2019-04-15
中文翻译:

在金黄色葡萄球菌骨髓炎期间,MyD88 和 IL-1R 信号驱动抗菌免疫和破骨细胞驱动的骨质流失。
金黄色葡萄球菌几乎能够感染所有器官系统,并且是骨髓炎(一种常见且使人衰弱的骨侵袭性感染)的常见分离病原体。骨髓炎的治疗需要侵入性外科手术和长期抗生素治疗,但由于病原体引起的广泛骨损伤会限制抗生素渗透和免疫细胞流入感染灶,因此治疗常常不成功。我们之前确定,金黄色葡萄球菌在小鼠骨髓炎模型中引发骨重塑的深刻改变,部分是通过产生溶骨毒素来实现的。然而,缺乏溶骨毒素的葡萄球菌菌株仍然会引起显着的骨质破坏,这表明宿主免疫反应也是骨髓炎期间病理性骨重塑的主要驱动因素。本研究的目的是确定金黄色葡萄球菌骨髓炎期间有助于抗菌免疫的宿主免疫途径,并确定这些免疫反应如何改变骨稳态并导致骨破坏。鉴于该信号通路在抗菌免疫和骨免疫串扰中的突出作用,我们特别关注白细胞介素 1 受体 (IL-1R) 和下游接头蛋白 MyD88。我们发现,虽然 IL-1R 信号传导对于骨髓炎期间细菌复制的局部控制是必要的,但它也会导致感染期间的骨质流失。从机制上讲,我们证明金黄色葡萄球菌在体外增强骨髓前体的破骨细胞生成,并在体内增加驻留在骨表面的破骨细胞的丰度。这种增强的破骨细胞丰度会导致小梁骨丢失,并且依赖于完整的 IL-1R 信号传导。 总的来说,这些数据将 IL-1R 信号传导定义为宿主对金黄色葡萄球菌骨髓炎反应的关键组成部分,但也证明 IL-1R 依赖性免疫反应通过激活破骨细胞介导的骨吸收触发附带骨损伤。





























 京公网安备 11010802027423号
京公网安备 11010802027423号