当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Pediatric CLIF-SOFA score is the best predictor of 28-day mortality in children with decompensated chronic liver disease
Journal of Hepatology ( IF 26.8 ) Pub Date : 2018-03-01 , DOI: 10.1016/j.jhep.2017.10.001 Rishi Bolia , Anshu Srivastava , Surender Kumar Yachha , Ujjal Poddar
Journal of Hepatology ( IF 26.8 ) Pub Date : 2018-03-01 , DOI: 10.1016/j.jhep.2017.10.001 Rishi Bolia , Anshu Srivastava , Surender Kumar Yachha , Ujjal Poddar
|
BACKGROUND & AIMS
Early identification of children with decompensated chronic liver disease (DCLD) at risk of short-term mortality helps improve outcome. We aimed to evaluate the predictors of outcome and role of Child-Pugh, pediatric end-stage liver disease (PELD) and pediatric chronic liver failure sequential organ failure assessment (pCLIF-SOFA) score for prognosticating 28-day mortality in children with DCLD. METHODS
DCLD children were prospectively evaluated with a clinico-laboratory proforma and followed for 28 days to determine outcome. Child-Pugh, PELD and pCLIF-SOFA were calculated at admission. Univariate and multivariate analysis was performed to identify the best predictors of outcome. RESULTS
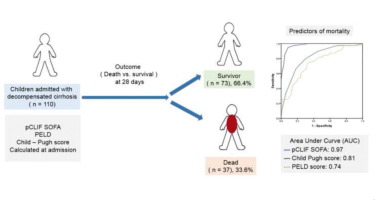
A total of 110 children (74 boys, 96 [4-204] months) were enrolled and 37 (33.6%) died at 28 days. Significant risk factors for mortality were a higher international normalized ratio (hazard ratio [HR] 1.17; 95% CI 1.04-1.31; p <0.001) and bilirubin (HR 1.04; 95% CI 1.01-1.08; p <0.001), lower albumin (HR 0.46; 95% CI 0.27-0.77; p = 0.03) and sodium (HR 0.93; 95% CI 0.89-0.98; p = 0.01), absence of treatable etiology (HR 2.00; 95% CI 1.40-2.87; p = 0.001) and presence of organ failure (HR 3.22; 95% CI 1.98-10.58; p <0.001). Organ failure and serum sodium were independent predictors of poor outcome on multivariate analysis. pCLIF-SOFA (16 [9-22] vs. 9 [5-15]), Child-Pugh (11 [9-15] vs. 10 [8-14]) and PELD (22.2 [7.5-45.3] vs. 15.3 [4.5-23.9]) scores were significantly higher in non-survivors. The area under the curve was 0.977 for pCLIF-SOFA, 0.815 for Child-Pugh score, and 0.741 for PELD score. A pCLIF-SOFA score of ≥11 identified 28-day mortality with a sensitivity and specificity of 94.9% and 91.5%, respectively. CONCLUSION
Thirty-four percent of children with DCLD have a poor short-term outcome. Organ failure and low serum sodium are independent predictors of outcome. pCLIF-SOFA performs better than Child-Pugh and PELD in prognostication of 28-day mortality. Our study supports the use of scores based on organ failure in prognosticating children with DCLD. LAY SUMMARY
The ability to predict the course of a disease is an important part of the assessment, enabling timely interventions that improve outcomes. We evaluated the outcome (death vs. survival) and compared three different scoring systems for their ability to predict mortality within 28 days in children with decompensated chronic liver disease (DCLD). One-third of children with DCLD died within 28 days and the pediatric chronic liver failure sequential organ failure assessment score, which considers the main organ systems of the body (lungs, liver, brain, kidney, blood and cardiac) fared better for identification of children with a poor outcome than the Child-Pugh and pediatric end-stage liver disease score which comprise of only liver-related parameters. Our study supports the use of scores based on organ failure in prognosticating children with DCLD.
中文翻译:

儿科 CLIF-SOFA 评分是失代偿期慢性肝病患儿 28 天死亡率的最佳预测指标
背景和目的 早期识别有短期死亡风险的失代偿性慢性肝病 (DCLD) 儿童有助于改善预后。我们旨在评估 Child-Pugh、儿科终末期肝病 (PELD) 和儿科慢性肝衰竭序贯器官衰竭评估 (pCLIF-SOFA) 评分对预测 DCLD 儿童 28 天死亡率的结果和作用的预测因子。方法 DCLD 儿童通过临床实验室形式进行前瞻性评估,并随访 28 天以确定结果。Child-Pugh、PELD 和 pCLIF-SOFA 在入院时计算。进行单变量和多变量分析以确定结果的最佳预测因子。结果 共纳入 110 名儿童(74 名男孩,96 [4-204] 个月),37 名(33.6%)在 28 天时死亡。死亡的重要危险因素是较高的国际标准化比率(风险比 [HR] 1.17;95% CI 1.04-1.31;p <0.001)和胆红素(HR 1.04;95% CI 1.01-1.08;p <0.001)、较低的白蛋白(HR 0.46;95% CI 0.27-0.77;p = 0.03)和钠(HR 0.93;95% CI 0.89-0.98;p = 0.01),缺乏可治疗的病因(HR 2.00;95% CI 1.40-2.87) 0.001)和器官衰竭的存在(HR 3.22;95% CI 1.98-10.58;p <0.001)。器官衰竭和血清钠是多变量分析结果不良的独立预测因素。pCLIF-SOFA (16 [9-22] vs. 9 [5-15])、Child-Pugh (11 [9-15] vs. 10 [8-14]) 和 PELD (22.2 [7.5-45.3] vs. 15.3 [4.5-23.9]) 分数在非幸存者中显着更高。pCLIF-SOFA 的曲线下面积为 0.977,Child-Pugh 评分为 0.815,PELD 评分为 0.741。pCLIF-SOFA 评分≥11 可确定 28 天死亡率,敏感性和特异性分别为 94.9% 和 91.5%。结论 34% 的 DCLD 儿童短期预后不佳。器官衰竭和低血清钠是结果的独立预测因子。pCLIF-SOFA 在预测 28 天死亡率方面的表现优于 Child-Pugh 和 PELD。我们的研究支持使用基于器官衰竭的评分来预测 DCLD 儿童。概述 预测疾病进程的能力是评估的重要组成部分,能够及时干预以改善结果。我们评估了结果(死亡与存活),并比较了三种不同评分系统预测失代偿性慢性肝病 (DCLD) 儿童 28 天内死亡率的能力。三分之一的 DCLD 儿童在 28 天内死亡,并且考虑身体主要器官系统(肺、肝、脑、肾、血液和心脏)的儿科慢性肝衰竭序贯器官衰竭评估评分在识别疾病方面表现更好与仅包含肝脏相关参数的 Child-Pugh 和儿科终末期肝病评分相比,预后较差的儿童。我们的研究支持使用基于器官衰竭的评分来预测 DCLD 儿童。血液和心脏)比仅包含肝脏相关参数的 Child-Pugh 和儿科终末期肝病评分在识别预后不良的儿童方面表现更好。我们的研究支持使用基于器官衰竭的评分来预测 DCLD 儿童。血液和心脏)比仅包含肝脏相关参数的 Child-Pugh 和儿科终末期肝病评分在识别预后不良的儿童方面表现更好。我们的研究支持使用基于器官衰竭的评分来预测 DCLD 儿童。
更新日期:2018-03-01
中文翻译:

儿科 CLIF-SOFA 评分是失代偿期慢性肝病患儿 28 天死亡率的最佳预测指标
背景和目的 早期识别有短期死亡风险的失代偿性慢性肝病 (DCLD) 儿童有助于改善预后。我们旨在评估 Child-Pugh、儿科终末期肝病 (PELD) 和儿科慢性肝衰竭序贯器官衰竭评估 (pCLIF-SOFA) 评分对预测 DCLD 儿童 28 天死亡率的结果和作用的预测因子。方法 DCLD 儿童通过临床实验室形式进行前瞻性评估,并随访 28 天以确定结果。Child-Pugh、PELD 和 pCLIF-SOFA 在入院时计算。进行单变量和多变量分析以确定结果的最佳预测因子。结果 共纳入 110 名儿童(74 名男孩,96 [4-204] 个月),37 名(33.6%)在 28 天时死亡。死亡的重要危险因素是较高的国际标准化比率(风险比 [HR] 1.17;95% CI 1.04-1.31;p <0.001)和胆红素(HR 1.04;95% CI 1.01-1.08;p <0.001)、较低的白蛋白(HR 0.46;95% CI 0.27-0.77;p = 0.03)和钠(HR 0.93;95% CI 0.89-0.98;p = 0.01),缺乏可治疗的病因(HR 2.00;95% CI 1.40-2.87) 0.001)和器官衰竭的存在(HR 3.22;95% CI 1.98-10.58;p <0.001)。器官衰竭和血清钠是多变量分析结果不良的独立预测因素。pCLIF-SOFA (16 [9-22] vs. 9 [5-15])、Child-Pugh (11 [9-15] vs. 10 [8-14]) 和 PELD (22.2 [7.5-45.3] vs. 15.3 [4.5-23.9]) 分数在非幸存者中显着更高。pCLIF-SOFA 的曲线下面积为 0.977,Child-Pugh 评分为 0.815,PELD 评分为 0.741。pCLIF-SOFA 评分≥11 可确定 28 天死亡率,敏感性和特异性分别为 94.9% 和 91.5%。结论 34% 的 DCLD 儿童短期预后不佳。器官衰竭和低血清钠是结果的独立预测因子。pCLIF-SOFA 在预测 28 天死亡率方面的表现优于 Child-Pugh 和 PELD。我们的研究支持使用基于器官衰竭的评分来预测 DCLD 儿童。概述 预测疾病进程的能力是评估的重要组成部分,能够及时干预以改善结果。我们评估了结果(死亡与存活),并比较了三种不同评分系统预测失代偿性慢性肝病 (DCLD) 儿童 28 天内死亡率的能力。三分之一的 DCLD 儿童在 28 天内死亡,并且考虑身体主要器官系统(肺、肝、脑、肾、血液和心脏)的儿科慢性肝衰竭序贯器官衰竭评估评分在识别疾病方面表现更好与仅包含肝脏相关参数的 Child-Pugh 和儿科终末期肝病评分相比,预后较差的儿童。我们的研究支持使用基于器官衰竭的评分来预测 DCLD 儿童。血液和心脏)比仅包含肝脏相关参数的 Child-Pugh 和儿科终末期肝病评分在识别预后不良的儿童方面表现更好。我们的研究支持使用基于器官衰竭的评分来预测 DCLD 儿童。血液和心脏)比仅包含肝脏相关参数的 Child-Pugh 和儿科终末期肝病评分在识别预后不良的儿童方面表现更好。我们的研究支持使用基于器官衰竭的评分来预测 DCLD 儿童。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号