JAMA Psychiatry ( IF 22.5 ) Pub Date : 2017-08-02 , DOI: 10.1001/jamapsychiatry.2017.2150 Martina de Zwaan 1 , Stephan Herpertz 2 , Stephan Zipfel 3 , Jennifer Svaldi 4 , Hans-Christoph Friederich 5 , Frauke Schmidt 1 , Andreas Mayr 6 , Tony Lam 7 , Carmen Schade-Brittinger 8 , Anja Hilbert 9
|
Importance Although cognitive behavioral therapy (CBT) represents the criterion standard for treatment of binge eating disorder (BED), most individuals do not have access to this specialized treatment.
Objective To evaluate the efficacy of internet-based guided self-help (GSH-I) compared with traditional, individual face-to-face CBT.
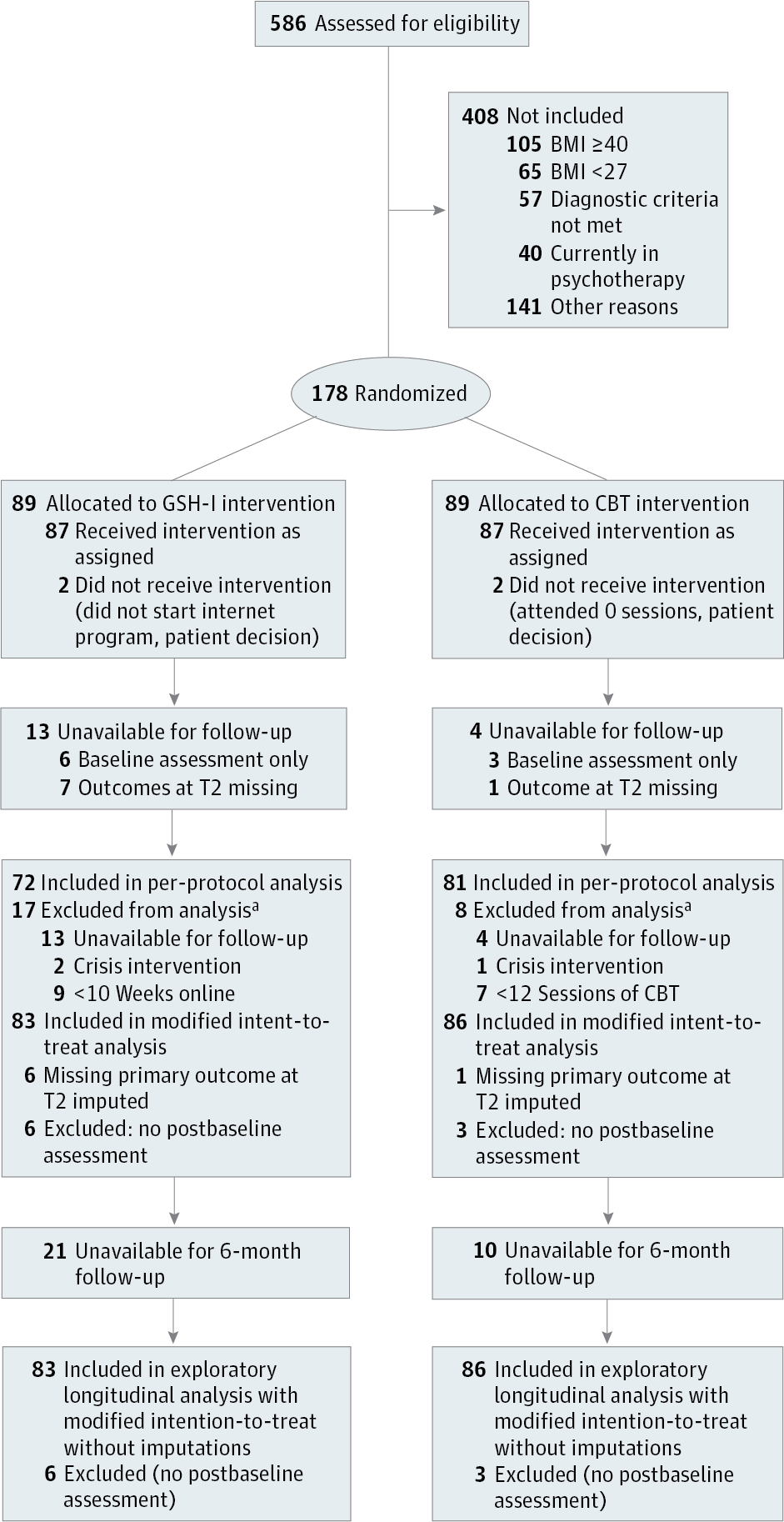
Design, Setting, and Participants The Internet and Binge Eating Disorder (INTERBED) study is a prospective, multicenter, randomized, noninferiority clinical trial (treatment duration, 4 months; follow-ups, 6 months and 1.5 years). A volunteer sample of 178 adult outpatients with full or subsyndromal BED were recruited from 7 university-based outpatient clinics from August 1, 2010, through December 31, 2011; final follow-up assessment was in April 2014. Data analysis was performed from November 30, 2014, to May 27, 2015.
Interventions Participants received 20 individual face-to-face CBT sessions of 50 minutes each or sequentially completed 11 internet modules and had weekly email contacts.
Main Outcomes and Measures The primary outcome was the difference in the number of days with objective binge eating episodes (OBEs) during the previous 28 days between baseline and end of treatment. Secondary outcomes included OBEs at follow-ups, eating disorder and general psychopathologic findings, body mass index, and quality of life.
Results A total of 586 patients were screened, 178 were randomized, and 169 had at least one postbaseline assessment and constituted the modified intention-to-treat analysis group (mean [SD] age, 43.2 [12.3] years; 148 [87.6%] female); the 1.5-year follow-up was available in 116 patients. The confirmatory analysis using the per-protocol sample (n = 153) failed to show noninferiority of GSH-I (adjusted effect, 1.47; 95% CI, −0.01 to 2.91; P = .05). Using the modified intention-to-treat sample, GSH-I was inferior to CBT in reducing OBE days at the end of treatment (adjusted effect, 1.63; 95% CI, 0.17-3.05; P = .03). Exploratory longitudinal analyses also showed the superiority of CBT over GSH-I by the 6-month (adjusted effect, 0.36; 95% CI, 0.23-0.55; P < .001) but not the 1.5-year follow-up (adjusted effect, 0.91; 95% CI, 0.54-1.50; P = .70). Reductions in eating disorder psychopathologic findings were significantly higher in the CBT group than in the GSH-I group at 6-month follow-up (adjusted effect, −0.4; 95% CI, −0.68 to −0.13; P = .005). No group differences were found for body mass index, general psychopathologic findings, and quality of life.
Conclusions and Relevance Face-to-face CBT leads to quicker and greater reductions in the number of OBE days, abstinence rates, and eating disorder psychopathologic findings and may be a better initial treatment option than GSH-I. Internet-based guided self-help remains a viable, slower-acting, low-threshold treatment alternative compared with CBT for adults with BED.
Trial Registration isrctn.org Identifier: ISRCTN40484777 and germanctr.de Identifier: DRKS00000409
中文翻译:

基于互联网的引导式自助服务与个人面对面治疗对超重或肥胖患者完全或亚综合征暴饮暴食症的影响INTERBED随机临床试验
重要性 尽管认知行为疗法(CBT)代表了暴食症(BED)的治疗标准,但大多数人无法获得这种专门的治疗。
目的 评估与传统的个人面对面CBT相比,基于Internet的自助服务(GSH-I)的疗效。
设计,环境和参与者 互联网和暴饮暴食症(INTERBED)研究是一项前瞻性,多中心,随机,非劣效性临床试验(治疗时间4个月;随访6个月和1.5年)。从2010年8月1日至2011年12月31日,从7家大学门诊诊所招募了178名成年BED完全或亚综合征的成人门诊患者。最终的后续评估于2014年4月进行。数据分析时间为2014年11月30日至2015年5月27日。
干预 参与者参加了20个单独的面对面的CBT会话,每个会话50分钟,或者依次完成了11个互联网模块,并每周进行电子邮件联系。
主要结果和措施 主要结果是基线和治疗结束之间的前28天,客观暴饮暴食发作(OBE)的天数差异。次要结果包括随访时的OBE,进食障碍和一般的心理病理发现,体重指数和生活质量。
结果 共筛选了586例患者,随机分组的178例,至少有一项基线后评估的169例,构成了改良的意向性治疗分析组(平均[SD]年龄,43.2 [12.3]岁; 148 [87.6%])女性); 对116例患者进行了1.5年的随访。使用基于方案的样本(n = 153)进行的确认分析未能显示GSH-1的非劣效性(调整后的效应为1.47; 95%CI为-0.01至2.91;P = 0.05)。使用改良的意向性治疗样品,在治疗结束时,GSH-1在减少OBE天数方面不如CBT(校正效应,1.63; 95%CI,0.17-3.05;P = .03)。探索性纵向分析还显示,到6个月时,CBT优于GSH-1(调整后的效果为0.36; 95%CI为0.23-0.55;P <.001),但不包括1.5年的随访(校正效应,0.91; 95%CI,0.54-1.50;P = .70)。在6个月的随访中,CBT组饮食失调的精神病理学发现明显高于GSH-I组(调整后的影响为-0.4; 95%CI为-0.68至-0.13;P = 0.005)。体重指数,一般精神病理学发现和生活质量没有发现群体差异。
结论和相关性 面对面的CBT可以更快,更大程度地减少OBE天数,节制率和进食障碍的精神病理学发现,并且可能是比GSH-I更好的初始治疗选择。与CBT相比,基于互联网的引导自助服务仍然是可行的,作用较慢的低阈值治疗方案,适用于患有BED的成人。
试用注册 isrctn.org标识符:ISRCTN40484777和germanctr.de标识符:DRKS00000409































 京公网安备 11010802027423号
京公网安备 11010802027423号