当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
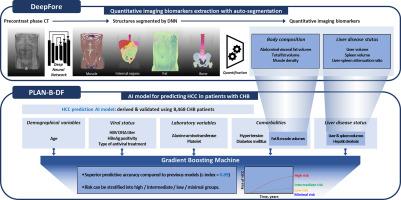
AI model using CT-based imaging biomarkers to predict hepatocellular carcinoma in patients with chronic hepatitis B
Journal of Hepatology ( IF 26.8 ) Pub Date : 2024-12-20 , DOI: 10.1016/j.jhep.2024.12.029 Hyunjae Shin, Moon Haeng Hur, Byeong Geun Song, Soo Young Park, Gi-Ae Kim, Gwang Hyun Choi, Joon Yeul Nam, Minseok Albert Kim, Youngsu Park, Yunmi Ko, Jeayeon Park, Han Ah Lee, Sung Won Chung, Na Ryung Choi, Min Kyung Park, Yun Bin Lee, Dong Hyun Sinn, Seung Up Kim, Hwi Young Kim, Jong-Min Kim, Jeong-Hoon Lee
更新日期:2024-12-20
Journal of Hepatology ( IF 26.8 ) Pub Date : 2024-12-20 , DOI: 10.1016/j.jhep.2024.12.029 Hyunjae Shin, Moon Haeng Hur, Byeong Geun Song, Soo Young Park, Gi-Ae Kim, Gwang Hyun Choi, Joon Yeul Nam, Minseok Albert Kim, Youngsu Park, Yunmi Ko, Jeayeon Park, Han Ah Lee, Sung Won Chung, Na Ryung Choi, Min Kyung Park, Yun Bin Lee, Dong Hyun Sinn, Seung Up Kim, Hwi Young Kim, Jong-Min Kim, Jeong-Hoon Lee
|






























 京公网安备 11010802027423号
京公网安备 11010802027423号