当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
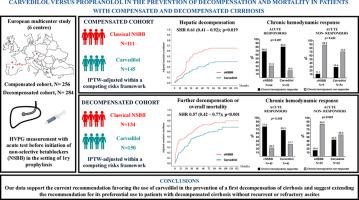
Carvedilol vs. propranolol for the prevention of decompensation and mortality in patients with compensated and decompensated cirrhosis
Journal of Hepatology ( IF 26.8 ) Pub Date : 2024-12-17 , DOI: 10.1016/j.jhep.2024.12.017 Jose Ignacio Fortea, Edilmar Alvarado-Tapias, Benedikt Simbrunner, Iranzu Ezcurra, Virginia Hernández-Gea, Carles Aracil, Elba Llop, Angela Puente, Cristina Roig, Thomas Reiberger, Juan Carlos García-Pagan, José Luis Calleja, Andreu Ferrero-Gregori, Matthias Mandorfer, Candid Villanueva, Javier Crespo
中文翻译:

卡维地洛与普萘洛尔预防代偿期和失代偿期肝硬化患者失代偿期和死亡率的比较
关于经典非选择性 β 受体阻滞剂(cNSBB,即普萘洛尔和纳多洛尔)与卡维地洛在肝硬化患者中的有效性的数据很少。本研究旨在比较它们预防代偿期和失代偿期肝硬化患者失代偿和死亡的潜力。
多中心回顾性研究,包括具有临床意义的门静脉高压症的代偿期和非代偿期肝硬化患者,接受肝静脉压梯度 (HVPG) 测量以评估静脉注射普萘洛尔的急性血流动力学反应(即 HVPG 从基线值降低 ≥10%)在静脉曲张出血的初步预防之前。在竞争风险框架中使用治疗加权的逆概率 (IPTW) 调整结局。
共纳入 540 例肝硬化患者,其中 256 例代偿期 (cNSBB n=111;卡维地洛 n=145) 和 284 例失代偿期 (cNSBB n=134;卡维地洛 n=150)。中位随访分别为 36.3 (IQR 16.9-61.0) 个月和 30.7 (IQR 13.1-52.2) 个月。在与 IPTW 进行协变量平衡后,与 cNSBB 相比,卡维地洛显著降低了代偿患者首次失代偿的风险(SHR 0.61;95% CI 0.41-0.92;p=0.019)和失代偿患者进一步失代偿/死亡的联合终点(SHR 0.57;95% CI 0.42-0.77;p<0.0001)。对 176 例 (68.8%,代偿) 和 177 例患者 (62.3%,失代偿) 进行了第二次 HVPG。急性无反应者,包括代偿期 (11.1% vs. 29.4%;p=0.422) 和失代偿期 (16.0% vs. 43.6%: p=0.0247) 患者,显示卡维地洛达到慢性血流动力学反应的可能性更高。两种 NSBB 的安全性在两个队列中均具有可比性。
我们的数据支持目前支持使用卡维地洛预防肝硬化首次失代偿的建议,并建议将其优先使用的建议扩展到无复发性或难治性腹水的失代偿期肝硬化患者。
本研究解决了经典非选择性 β 受体阻滞剂(例如普萘洛尔和纳多洛尔)与卡维地洛在代偿期和非代偿期肝硬化治疗效果方面的比较效果差距。我们的结果支持在这两种情况下优先使用卡维地洛,因为它在减少首次和进一步失代偿方面具有卓越的疗效。然而,该研究的回顾性和固有的选择偏倚建议谨慎,不要将这些发现广泛应用于表现出循环功能障碍或复发性/难治性腹水迹象的失代偿期肝硬化患者。
更新日期:2024-12-17
Journal of Hepatology ( IF 26.8 ) Pub Date : 2024-12-17 , DOI: 10.1016/j.jhep.2024.12.017 Jose Ignacio Fortea, Edilmar Alvarado-Tapias, Benedikt Simbrunner, Iranzu Ezcurra, Virginia Hernández-Gea, Carles Aracil, Elba Llop, Angela Puente, Cristina Roig, Thomas Reiberger, Juan Carlos García-Pagan, José Luis Calleja, Andreu Ferrero-Gregori, Matthias Mandorfer, Candid Villanueva, Javier Crespo
|
Background and Aims
Data on the effectiveness of classical non-selective beta-blockers (cNSBB, i.e., propranolol and nadolol) versus carvedilol in patients with cirrhosis are scarce. The present study aimed to compare their potential for preventing decompensation and mortality in patients with compensated and decompensated cirrhosis.Methods
Multicenter retrospective study including compensated and decompensated cirrhotic patients with clinically significant portal hypertension, undergoing measurement of hepatic venous pressure gradient (HVPG) to assess acute hemodynamic response to intravenous propranolol (i.e., HVPG decrease≥10% from baseline value) prior to primary prophylaxis for variceal bleeding. Outcomes were adjusted using Inverse Probability of Treatment Weighting (IPTW) in a competitive risk framework.Results
A total of 540 patients with cirrhosis were included, 256 compensated (cNSBB n=111; carvedilol n=145) and 284 decompensated (cNSBB n=134; carvedilol n=150). Median follow-up was 36.3 (IQR 16.9-61.0) months and 30.7 (IQR 13.1-52.2) months, respectively. After covariate balancing with IPTW, carvedilol, compared to cNSBB, significantly reduced the risk of a first decompensation in compensated patients (SHR 0.61; 95% CI 0.41-0.92; p=0.019) and a combined endpoint of further decompensation/death in decompensated patients (SHR 0.57; 95% CI 0.42-0.77; p<0.0001). A second HVPG was conducted on 176 (68.8%, compensated) and 177 patients (62.3%, decompensated). Acute non-responders, both compensated (11.1% vs. 29.4%; p=0.422) and decompensated (16.0% vs. 43.6%: p=0.0247) patients, showed a higher likelihood of achieving a chronic hemodynamic response with carvedilol. The safety profile of each type of NSBB was comparable in both cohorts.Conclusions
Our data endorse the current recommendation favoring the use of carvedilol in the prevention of a first decompensation of cirrhosis and suggest extending the recommendation for its preferential use to patients with decompensated cirrhosis without recurrent or refractory ascites.IMPACT AND IMPLICATIONS
This study addresses a gap in the comparative effectiveness of classical non-selective beta-blockers (e.g., propranolol and nadolol) versus carvedilol in managing cirrhosis in both compensated and decompensated stages. Our results support the preferential use of carvedilol in both settings due to its superior efficacy in reducing first and further decompensation. However, the retrospective nature of the study and inherent selection biases advise caution against broadly applying these findings to patients with decompensated cirrhosis who exhibit signs of circulatory dysfunction or recurrent/refractory ascites.中文翻译:

卡维地洛与普萘洛尔预防代偿期和失代偿期肝硬化患者失代偿期和死亡率的比较
背景和目标
关于经典非选择性 β 受体阻滞剂(cNSBB,即普萘洛尔和纳多洛尔)与卡维地洛在肝硬化患者中的有效性的数据很少。本研究旨在比较它们预防代偿期和失代偿期肝硬化患者失代偿和死亡的潜力。
方法
多中心回顾性研究,包括具有临床意义的门静脉高压症的代偿期和非代偿期肝硬化患者,接受肝静脉压梯度 (HVPG) 测量以评估静脉注射普萘洛尔的急性血流动力学反应(即 HVPG 从基线值降低 ≥10%)在静脉曲张出血的初步预防之前。在竞争风险框架中使用治疗加权的逆概率 (IPTW) 调整结局。
结果
共纳入 540 例肝硬化患者,其中 256 例代偿期 (cNSBB n=111;卡维地洛 n=145) 和 284 例失代偿期 (cNSBB n=134;卡维地洛 n=150)。中位随访分别为 36.3 (IQR 16.9-61.0) 个月和 30.7 (IQR 13.1-52.2) 个月。在与 IPTW 进行协变量平衡后,与 cNSBB 相比,卡维地洛显著降低了代偿患者首次失代偿的风险(SHR 0.61;95% CI 0.41-0.92;p=0.019)和失代偿患者进一步失代偿/死亡的联合终点(SHR 0.57;95% CI 0.42-0.77;p<0.0001)。对 176 例 (68.8%,代偿) 和 177 例患者 (62.3%,失代偿) 进行了第二次 HVPG。急性无反应者,包括代偿期 (11.1% vs. 29.4%;p=0.422) 和失代偿期 (16.0% vs. 43.6%: p=0.0247) 患者,显示卡维地洛达到慢性血流动力学反应的可能性更高。两种 NSBB 的安全性在两个队列中均具有可比性。
结论
我们的数据支持目前支持使用卡维地洛预防肝硬化首次失代偿的建议,并建议将其优先使用的建议扩展到无复发性或难治性腹水的失代偿期肝硬化患者。
影响和影响
本研究解决了经典非选择性 β 受体阻滞剂(例如普萘洛尔和纳多洛尔)与卡维地洛在代偿期和非代偿期肝硬化治疗效果方面的比较效果差距。我们的结果支持在这两种情况下优先使用卡维地洛,因为它在减少首次和进一步失代偿方面具有卓越的疗效。然而,该研究的回顾性和固有的选择偏倚建议谨慎,不要将这些发现广泛应用于表现出循环功能障碍或复发性/难治性腹水迹象的失代偿期肝硬化患者。






























 京公网安备 11010802027423号
京公网安备 11010802027423号