当前位置:
X-MOL 学术
›
Am. J. Hematol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Clinical significance of complete remission and measurable residual disease in relapsed/refractory multiple myeloma patients treated with T‐cell redirecting immunotherapy
American Journal of Hematology ( IF 10.1 ) Pub Date : 2024-11-16 , DOI: 10.1002/ajh.27526 Aintzane Zabaleta, Noemi Puig, Maria‐Teresa Cedena, Aina Oliver‐Caldes, José J. Perez, Cristina Moreno, Luis‐Esteban Tamariz‐Amador, Paula Rodriguez‐Otero, Felipe Prosper, Veronica Gonzalez‐Calle, Lucía López‐Corral, Beatriz Rey‐Búa, Borja Puertas, Fátima Mirás, José María Sánchez‐Pina, Nieves López‐Muñoz, Manel Juan, E. Azucena González‐Navarro, Álvaro Urbano, Carlos Fernández de Larrea, Joan Blade, Juan‐José Lahuerta, Joaquín Martinez‐Lopez, Maria‐Victoria Mateos, Jesús F. San Miguel, Bruno Paiva
American Journal of Hematology ( IF 10.1 ) Pub Date : 2024-11-16 , DOI: 10.1002/ajh.27526 Aintzane Zabaleta, Noemi Puig, Maria‐Teresa Cedena, Aina Oliver‐Caldes, José J. Perez, Cristina Moreno, Luis‐Esteban Tamariz‐Amador, Paula Rodriguez‐Otero, Felipe Prosper, Veronica Gonzalez‐Calle, Lucía López‐Corral, Beatriz Rey‐Búa, Borja Puertas, Fátima Mirás, José María Sánchez‐Pina, Nieves López‐Muñoz, Manel Juan, E. Azucena González‐Navarro, Álvaro Urbano, Carlos Fernández de Larrea, Joan Blade, Juan‐José Lahuerta, Joaquín Martinez‐Lopez, Maria‐Victoria Mateos, Jesús F. San Miguel, Bruno Paiva
|
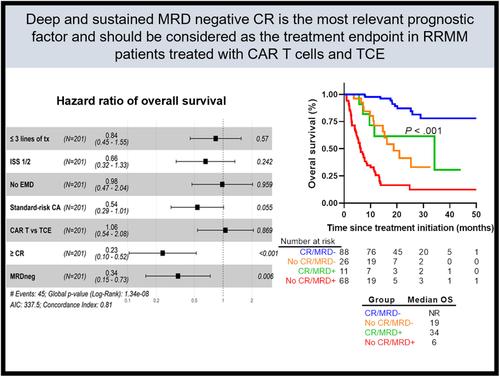
The impact of measurable residual disease (MRD) in relapse/refractory multiple myeloma (RRMM) patients treated with T‐cell redirecting immunotherapy is uncertain. We analyzed MRD dynamics using next‐generation flow in 201 patients treated in clinical trials with chimeric antigen receptor (CAR) T cells and T‐cell engagers (TCE). Achieving MRD negativity at 10−6 was associated with 89% reduction in the risk of progression and/or death. Survival outcomes were improved in patients with sustained versus transient MRD negativity and were dismal in those who remained MRD positive. The intent‐to‐treat MRD negative rates were higher in patients treated with CAR T cells versus TCE. However, among patients achieving MRD negativity, there were no differences in survival outcomes when stratified according to treatment with CAR T cells versus TCE. In multivariate analysis including the number of prior lines of treatment, International Staging System, cytogenetic risk, extramedullary disease and type of T‐cell redirecting immunotherapy, only the complete remission (CR) and MRD statuses showed independent prognostic value for progression‐free and overall survival. In conclusion, our study shows that deep and sustained MRD negative CR is the most relevant prognostic factor and should be considered as the treatment endpoint in RRMM patients treated with CAR T cells and TCE.
中文翻译:

接受 T 细胞重定向免疫治疗的复发/难治性多发性骨髓瘤患者完全缓解和可测量残留病灶的临床意义
可测量残留病灶 (MRD) 对接受 T 细胞重定向免疫疗法治疗的复发/难治性多发性骨髓瘤 (RRMM) 患者的影响尚不确定。我们使用下一代血流分析了 201 例在临床试验中接受嵌合抗原受体 (CAR) T 细胞和 T 细胞接合器 (TCE) 治疗的患者的 MRD 动力学。达到 10-6 的 MRD 阴性与进展和/或死亡风险降低 89% 相关。与短暂性 MRD 阴性患者的生存结局相比,生存结局有所改善,而 MRD 保持阳性的患者的生存结局令人沮丧。与 TCE 相比,接受 CAR T 细胞治疗的患者意向治疗 MRD 阴性率更高。然而,在达到 MRD 阴性的患者中,根据 CAR T 细胞治疗与 TCE 治疗分层时,生存结果没有差异。在包括既往治疗线数量、国际分期系统、细胞遗传学风险、髓外疾病和 T 细胞重定向免疫疗法类型在内的多变量分析中,只有完全缓解 (CR) 和 MRD 状态对无进展生存期和总生存期显示出独立的预后价值。总之,我们的研究表明,深度和持续的 MRD 阴性 CR 是最相关的预后因素,应被视为接受 CAR T 细胞和 TCE 治疗的 RRMM 患者的治疗终点。
更新日期:2024-11-16
中文翻译:

接受 T 细胞重定向免疫治疗的复发/难治性多发性骨髓瘤患者完全缓解和可测量残留病灶的临床意义
可测量残留病灶 (MRD) 对接受 T 细胞重定向免疫疗法治疗的复发/难治性多发性骨髓瘤 (RRMM) 患者的影响尚不确定。我们使用下一代血流分析了 201 例在临床试验中接受嵌合抗原受体 (CAR) T 细胞和 T 细胞接合器 (TCE) 治疗的患者的 MRD 动力学。达到 10-6 的 MRD 阴性与进展和/或死亡风险降低 89% 相关。与短暂性 MRD 阴性患者的生存结局相比,生存结局有所改善,而 MRD 保持阳性的患者的生存结局令人沮丧。与 TCE 相比,接受 CAR T 细胞治疗的患者意向治疗 MRD 阴性率更高。然而,在达到 MRD 阴性的患者中,根据 CAR T 细胞治疗与 TCE 治疗分层时,生存结果没有差异。在包括既往治疗线数量、国际分期系统、细胞遗传学风险、髓外疾病和 T 细胞重定向免疫疗法类型在内的多变量分析中,只有完全缓解 (CR) 和 MRD 状态对无进展生存期和总生存期显示出独立的预后价值。总之,我们的研究表明,深度和持续的 MRD 阴性 CR 是最相关的预后因素,应被视为接受 CAR T 细胞和 TCE 治疗的 RRMM 患者的治疗终点。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号