当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
The Association of Hospital-Cardiologist Integration With Patient Outcomes, Care Quality, and Utilization
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2024-11-15 , DOI: 10.1016/j.jacc.2024.10.109 Ali Moghtaderi, David J. Magid, Andy Ye Yuan, Bernard Black, Qian (Eric) Luo, Vinay Kini
中文翻译:

医院-心脏病专家整合与患者结果、护理质量和利用率的关联
心脏病专家越来越多地从独立执业转向医院直接就业。医院就业有可能改善护理协调和交付,但对其对护理质量和结果的影响知之甚少。
在这项研究中,我们试图评估心脏病专家的医院就业与急性心肌梗死 (AMI) 或心力衰竭 (HF) 住院患者预后、护理质量和利用率之间的关联。
我们使用了 2008 年至 2019 年因 AMI 或 HF 事件住院的 Medicare 按服务收费受益人的样本。我们确定了照顾这些患者的负责任的心脏病专家,并通过税号确定他们的就业状况。我们使用双重差分法来比较从独立实践转变为医院雇佣的心脏病专家治疗的患者的临床结局、质量指标和利用率,以及由保持独立的心脏病专家治疗的患者的结局。根据时间趋势和患者、医院和心脏病专家特征调整模型。患者结局为院内死亡率、 30 天死亡率和 30 天再入院率。质量测量包括:1) 指南推荐的评估心脏功能的测试;2) 30 天的随访门诊就诊。利用指标是住院时间,对于 AMI 患者,接受冠状动脉血运重建的比例。
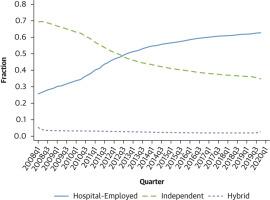
医院雇用的美国心脏病专家的比例从 2008 年的 26% 增加到 2019 年的 63%。我们确定了 186,052 名 AMI 和 259,849 名 HF 患者由转行医院工作的心脏病专家照顾,以及 168,052 名 AMI 和 245,769 名 HF 患者由独立心脏病专家照顾。患者特征相似 (平均年龄 80.8 岁;47% 为男性)。我们发现结局没有显著差异(例如,AMI 患者 30 天死亡率的调整差异为 0.03% [95% CI: -0.39%, 0.45%],HF 患者为 -0.05% [95% CI: -0.37%, 0.27%]);大多数质量指标没有差异,除了 30 天随访的 HF 患者比例略有增加(调整后的差异:1.04%;95% CI:0.46%-1.62%);由医院雇佣的心脏病专家 (postswitch) 治疗的患者与独立心脏病专家治疗的患者在利用率方面没有差异。
在美国心脏病专家中,已经从独立执业转变为医院直接就业。我们发现很少有证据表明医院雇用心脏病专家可以提高护理质量或结局。
更新日期:2024-11-15
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2024-11-15 , DOI: 10.1016/j.jacc.2024.10.109 Ali Moghtaderi, David J. Magid, Andy Ye Yuan, Bernard Black, Qian (Eric) Luo, Vinay Kini
|
Background
Cardiologists are increasingly moving from independent practice to direct employment by hospitals. Hospital employment has the potential to improve care coordination and delivery, but little is known about its effect on care quality and outcomes.Objectives
In this study, we sought to assess the association between hospital employment of cardiologists and patient outcomes, care quality, and utilization among patients hospitalized with incident acute myocardial infarction (AMI) or heart failure (HF).Methods
We used a sample of Medicare fee-for-service beneficiaries hospitalized with incident AMI or HF from 2008 to 2019. We identified the accountable cardiologists that cared for these patients and determined their employment status by means of tax identification numbers. We used difference-in-differences methods to compare clinical outcomes, quality measures, and utilization for patients treated by hospital-employed cardiologists after switching from independent to hospital-employed practice, to outcomes for patients treated by cardiologists who remained independent. Models were adjusted for time trends and patient, hospital, and cardiologist characteristics. Patient outcomes were in-hospital mortality, 30-day mortality, and 30-day readmission. Quality measures were receipt of: 1) a guideline-recommended test to assess cardiac function; and 2) a 30-day follow-up clinic visit. Utilization measures were length of stay and, for AMI patients, the proportion receiving coronary revascularization.Results
The proportion of U.S. cardiologists employed by hospitals increased from 26% in 2008 to 63% in 2019. We identified 186,052 AMI and 259,849 HF patients cared for by cardiologists who switched to hospital employment and 168,052 AMI and 245,769 HF patients cared for by independent cardiologists. Patient characteristics were similar (mean age 80.8 years; 47% men). We found no significant differences in outcomes (eg, adjusted difference in 30-day mortality 0.03% [95% CI: −0.39% to 0.45%] for AMI patients and −0.05% [95% CI: −0.37% to 0.27%] for HF patients); no differences in most quality metrics except a small increase in the proportion of HF patients with 30-day follow-up (adjusted difference: 1.04%; 95% CI: 0.46%-1.62%); and no differences in utilization between patients treated by hospital-employed cardiologists (postswitch) vs independent cardiologists.Conclusions
Among U.S. cardiologists, there has been a large shift from independent practice to direct employment by hospitals. We found minimal evidence that cardiologist employment by hospitals improves care quality or outcomes.中文翻译:

医院-心脏病专家整合与患者结果、护理质量和利用率的关联
背景
心脏病专家越来越多地从独立执业转向医院直接就业。医院就业有可能改善护理协调和交付,但对其对护理质量和结果的影响知之甚少。
目标
在这项研究中,我们试图评估心脏病专家的医院就业与急性心肌梗死 (AMI) 或心力衰竭 (HF) 住院患者预后、护理质量和利用率之间的关联。
方法
我们使用了 2008 年至 2019 年因 AMI 或 HF 事件住院的 Medicare 按服务收费受益人的样本。我们确定了照顾这些患者的负责任的心脏病专家,并通过税号确定他们的就业状况。我们使用双重差分法来比较从独立实践转变为医院雇佣的心脏病专家治疗的患者的临床结局、质量指标和利用率,以及由保持独立的心脏病专家治疗的患者的结局。根据时间趋势和患者、医院和心脏病专家特征调整模型。患者结局为院内死亡率、 30 天死亡率和 30 天再入院率。质量测量包括:1) 指南推荐的评估心脏功能的测试;2) 30 天的随访门诊就诊。利用指标是住院时间,对于 AMI 患者,接受冠状动脉血运重建的比例。
结果
医院雇用的美国心脏病专家的比例从 2008 年的 26% 增加到 2019 年的 63%。我们确定了 186,052 名 AMI 和 259,849 名 HF 患者由转行医院工作的心脏病专家照顾,以及 168,052 名 AMI 和 245,769 名 HF 患者由独立心脏病专家照顾。患者特征相似 (平均年龄 80.8 岁;47% 为男性)。我们发现结局没有显著差异(例如,AMI 患者 30 天死亡率的调整差异为 0.03% [95% CI: -0.39%, 0.45%],HF 患者为 -0.05% [95% CI: -0.37%, 0.27%]);大多数质量指标没有差异,除了 30 天随访的 HF 患者比例略有增加(调整后的差异:1.04%;95% CI:0.46%-1.62%);由医院雇佣的心脏病专家 (postswitch) 治疗的患者与独立心脏病专家治疗的患者在利用率方面没有差异。
结论
在美国心脏病专家中,已经从独立执业转变为医院直接就业。我们发现很少有证据表明医院雇用心脏病专家可以提高护理质量或结局。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号