当前位置:
X-MOL 学术
›
Eur. J. Heart Fail.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Long‐term clinical outcomes and healthcare resource utilization in male and female patients following hospitalization for heart failure
European Journal of Heart Failure ( IF 16.9 ) Pub Date : 2024-11-05 , DOI: 10.1002/ejhf.3499 Tauben Averbuch, Shun Fu Lee, Brandon Zagorski, Ambarish Pandey, Mark C. Petrie, Tor Biering‐Sorensen, Feng Xie, Harriette G.C. Van Spall
European Journal of Heart Failure ( IF 16.9 ) Pub Date : 2024-11-05 , DOI: 10.1002/ejhf.3499 Tauben Averbuch, Shun Fu Lee, Brandon Zagorski, Ambarish Pandey, Mark C. Petrie, Tor Biering‐Sorensen, Feng Xie, Harriette G.C. Van Spall
|
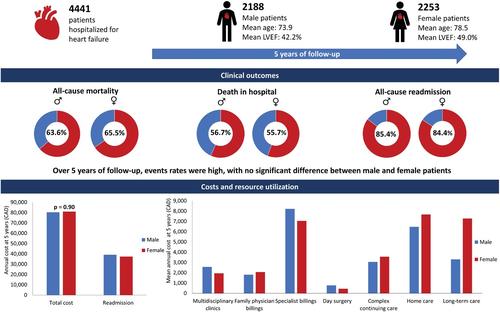
AimsHeart failure (HF ) is a leading cause of hospitalization, and sex differences in care have been described. We assessed sex‐specific clinical outcomes and healthcare resource utilization following hospitalization for HF. Methods and resultsThis was an exploratory analysis of patients hospitalized for HF across 10 Canadian hospitals in the Patient‐Centered Care Transitions in HF (PACT‐HF) cluster‐randomized trial. The primary outcome was all‐cause mortality. Secondary outcomes included all‐cause readmissions, HF readmissions, emergency department (ED) visits, and healthcare resource utilization. Outcomes were obtained via linkages with administrative datasets. Among 4441 patients discharged alive, 50.7% were female. By 5 years, 63.6% and 65.5% of male and female patients, respectively, had died (p = 0.19); 85.4% and 84.4%, respectively, were readmitted (p = 0.35); and 72.2% and 70.9%, respectively, received ED care without hospitalization (p = 0.34). There were no sex differences in mean [SD] number of all‐cause readmissions (males, 2.8 [7.8] and females, 3.0 [8.4], p = 0.54), HF readmissions (males, 0.9 [3.6] and females, 0.9 [4.5], p = 0.80), or ED visits (males, 1.8 [11.3] and females, 1.5 [6.0], p = 0.24) per person. There were no sex differences in mean [SD] annual direct healthcare cost per patient (males, $80 334 [116 762] versus females, $81 010 [112 625], p = 0.90), but males received more specialist, multidisciplinary HF clinic, haemodialysis, and day surgical care, and females received more home visits, continuing/convalescent care, and long‐term care. Annualized clinical events were highest in first year following index discharge in both males and females.ConclusionsAmong people discharged alive after hospitalization for HF, there were no sex differences in total and annual deaths, readmissions, and ED visits, or in total direct healthcare costs. Despite similar risk profiles, males received relatively more specialist care and day surgical procedures, and females received more supportive care.Clinical Trial Registration: ClinicalTrials.gov NCT02112227.
中文翻译:

男性和女性心力衰竭住院患者的远期临床结局和医疗资源利用
目的心力衰竭 (HF) 是住院的主要原因,并且已经描述了护理中的性别差异。我们评估了 HF 住院后性别特异性临床结局和医疗保健资源利用。方法和结果这是在以患者为中心的 HF 护理过渡 (PACT-HF) 整群随机试验中对加拿大 10 家医院因 HF 住院的患者进行的探索性分析。主要结局是全因死亡率。次要结局包括全因再入院、 HF 再入院、急诊科 (ED) 就诊和医疗保健资源利用。通过与行政数据集的联系获得结果。在 4441 名活着出院的患者中,50.7% 为女性。到 5 年时,男性和 65.5% 的患者分别死亡 (p = 0.19);分别有 85.4% 和 84.4% 再次入院 (p = 0.35);和 72.2% 和 70.9% 分别接受了 ED 护理而没有住院 (p = 0.34)。全因再入院的平均 [SD] 次数 (男性 2.8 [7.8] 和女性 3.0 [8.4],p = 0.54)、HF 再入院 (男性 0.9 [3.6] 和女性 0.9 [4.5],p = 0.80)或 ED 就诊 (男性,1.8 [11.3] 和女性,1.5 [6.0],p = 0.24)没有性别差异。每位患者的平均 [SD] 年度直接医疗保健费用 (男性 80 334 美元 [116 762] 与女性 81 010 美元 [112 625],p = 0.90)没有性别差异,但男性接受了更多的专科、多学科 HF 诊所、血液透析和日间手术护理,女性接受了更多的家访、持续/恢复护理和长期护理。男性和女性指数出院后第一年的年化临床事件最高。结论在 HF 住院后存活出院的人群中,总死亡人数和年度死亡人数、再入院人数和急诊就诊人数或总直接医疗保健费用没有性别差异。尽管风险相似,但男性接受了相对更多的专科护理和日间外科手术,而女性接受了更多的支持性护理。临床试验注册:ClinicalTrials.gov NCT02112227。
更新日期:2024-11-05
中文翻译:

男性和女性心力衰竭住院患者的远期临床结局和医疗资源利用
目的心力衰竭 (HF) 是住院的主要原因,并且已经描述了护理中的性别差异。我们评估了 HF 住院后性别特异性临床结局和医疗保健资源利用。方法和结果这是在以患者为中心的 HF 护理过渡 (PACT-HF) 整群随机试验中对加拿大 10 家医院因 HF 住院的患者进行的探索性分析。主要结局是全因死亡率。次要结局包括全因再入院、 HF 再入院、急诊科 (ED) 就诊和医疗保健资源利用。通过与行政数据集的联系获得结果。在 4441 名活着出院的患者中,50.7% 为女性。到 5 年时,男性和 65.5% 的患者分别死亡 (p = 0.19);分别有 85.4% 和 84.4% 再次入院 (p = 0.35);和 72.2% 和 70.9% 分别接受了 ED 护理而没有住院 (p = 0.34)。全因再入院的平均 [SD] 次数 (男性 2.8 [7.8] 和女性 3.0 [8.4],p = 0.54)、HF 再入院 (男性 0.9 [3.6] 和女性 0.9 [4.5],p = 0.80)或 ED 就诊 (男性,1.8 [11.3] 和女性,1.5 [6.0],p = 0.24)没有性别差异。每位患者的平均 [SD] 年度直接医疗保健费用 (男性 80 334 美元 [116 762] 与女性 81 010 美元 [112 625],p = 0.90)没有性别差异,但男性接受了更多的专科、多学科 HF 诊所、血液透析和日间手术护理,女性接受了更多的家访、持续/恢复护理和长期护理。男性和女性指数出院后第一年的年化临床事件最高。结论在 HF 住院后存活出院的人群中,总死亡人数和年度死亡人数、再入院人数和急诊就诊人数或总直接医疗保健费用没有性别差异。尽管风险相似,但男性接受了相对更多的专科护理和日间外科手术,而女性接受了更多的支持性护理。临床试验注册:ClinicalTrials.gov NCT02112227。






























 京公网安备 11010802027423号
京公网安备 11010802027423号