Diabetologia ( IF 8.4 ) Pub Date : 2024-11-04 , DOI: 10.1007/s00125-024-06295-1 Gillian L. Garden, Ka Siu Fan, Megan Paterson, Fariba Shojaee-Moradie, Monique Borg Inguanez, Antonios Manoli, Victoria Edwards, Vivienne Lee, Brian M. Frier, Ewan J. Hutchison, Declan Maher, Chantal Mathieu, Stuart J. Mitchell, Simon R. Heller, Graham A. Roberts, Kenneth M. Shaw, Gerd Koehler, Julia K. Mader, Bruce R. King, David L. Russell-Jones
|
Aims/hypothesis
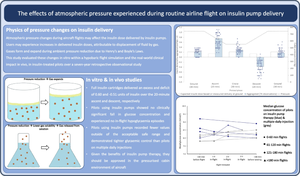
Glycaemic control and clinical outcomes in diabetes are improved by continuous subcutaneous insulin infusion (CSII). Atmospheric pressure changes during flights may affect insulin delivery from pumps and cause unintended metabolic consequences, including hypoglycaemia, in people with type 1 diabetes. The present report evaluates both hypobaric flight simulation and real-world data in pilots using insulin pumps while flying.
Methods
In the flight simulation part of this study, an in vitro study of insulin pumps was conducted in a hypobaric chamber, de-pressurised to 550 mmHg to mimic the atmospheric pressure changes in airliner cabins during commercial flights. Insulin delivery rates and bubble formation were recorded for standard flight protocol. Insulin infusion sets, without pumps, were tested in a simulated rapid decompression scenario. The real-world observational study was a 7.5-year retrospective cohort study in which pre- and in-flight self-monitored blood glucose (SMBG) values were monitored in pilots with insulin-treated diabetes. Commercial and private pilots granted a medical certificate to fly within the European Union Aviation Safety Agency approved protocol and receiving insulin either by pump or multiple daily injections (MDI) were included.
Results
In the flight simulation study, full cartridges over-delivered 0.60 U of insulin during a 20 min ascent and under-delivered by 0.51 U during descent compared with ground-level performance. During emergency rapid decompression, 5.6 U of excess insulin was delivered. In the real-world study, seven pilots using CSII recorded 4656 SMBG values during 2345 h of flying across 1081 flights. Only 33 (0.7%) values were outside an acceptable safe range (5.0–15.0 mmol/l [90–270 mg/dl]). No clinically significant fall in the median SMBG concentration was observed after aircraft ascent and no in-flight SMBG values were within the hypoglycaemic range (<4.0 mmol/l [<72 mg/dl]). Compared with pilots receiving MDI therapy, pilots using CSII recorded more SMBG values within the acceptable range (99.3% vs 97.5%), fewer values in the low red range (0.02% vs 0.1%), fewer in-flight out-of-range values (0.2% vs 1.3%) and maintained stricter glycaemic control during flight.
Conclusions/interpretation
Ambient pressure reduction during simulated flights results in bubble formation and expansion within insulin cartridges. This causes unintended delivery of small insulin doses independent of pre-determined delivery rates and represents the maximum amount of insulin that could be delivered and retracted. However, in vivo, pilots using CSII in-flight did not experience a fall in blood glucose or episodes of hypoglycaemia during these atmospheric pressure changes and the use of insulin pumps can be endorsed in view of their clinical benefits.
Graphical Abstract
中文翻译:

飞行过程中大气压力变化对胰岛素治疗糖尿病飞行员胰岛素泵输送和血糖控制的影响:体外模拟和回顾性观察性真实世界研究
目标/假设
持续皮下胰岛素输注 (CSII) 可改善糖尿病的血糖控制和临床结局。飞行过程中的大气压力变化可能会影响胰岛素泵的胰岛素输送,并导致 1 型糖尿病患者出现意外的代谢后果,包括低血糖。本报告评估了飞行员在飞行时使用胰岛素泵的低压飞行模拟和真实世界数据。
方法
在本研究的飞行模拟部分,胰岛素泵的体外研究是在低压室中进行的,减压至 550 mmHg,以模拟商业飞行期间客机机舱内的大气压力变化。记录标准飞行方案的胰岛素输送速率和气泡形成。在模拟快速减压场景中测试了不带泵的胰岛素输注器。真实世界观察性研究是一项为期 7.5 年的回顾性队列研究,其中监测了接受胰岛素治疗的糖尿病飞行员的飞行前和飞行中自我监测血糖 (SMBG) 值。商业和私人飞行员获得了医疗证明,可以在欧盟航空安全局批准的协议内飞行,并通过泵或每日多次注射 (MDI) 接受胰岛素。
结果
在飞行模拟研究中,与地面性能相比,满弹药筒在 20 分钟的上升过程中超额输送了 0.60 U 的胰岛素,在下降时低输了 0.51 U。在紧急快速减压期间,输送了 5.6 U 过量的胰岛素。在真实世界研究中,7 名使用 CSII 的飞行员在 1081 次飞行的 2345 小时飞行中记录了 4656 个 SMBG 值。只有 33 个 (0.7%) 值超出可接受的安全范围 (5.0-15.0 mmol/l [90-270 mg/dl])。飞机上升后未观察到中位 SMBG 浓度的临床显着下降,并且飞行中 SMBG 值在低血糖范围内 (<4.0 mmol/l [<72 mg/dl])。与接受 MDI 治疗的飞行员相比,使用 CSII 的飞行员在可接受范围内记录的 SMBG 值更高(99.3% 对 97.5%),红色低范围内的值更少(0.02% 对 0.1%),飞行中超出范围的值更少(0.2% 对 1.3%),并在飞行过程中保持更严格的血糖控制。
结论/解释
模拟飞行期间环境压力降低会导致胰岛素盒内形成气泡和膨胀。这会导致意外输送小剂量的胰岛素,与预先确定的输送速率无关,并且代表可以输送和回缩的最大胰岛素量。然而,在体内,在飞行中使用 CSII 的飞行员在这些大气压力变化期间没有出现血糖下降或低血糖发作,并且鉴于其临床益处,可以使用胰岛素泵。































 京公网安备 11010802027423号
京公网安备 11010802027423号