当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Blood markers for type-1,-2, and -3 inflammation are associated with severity of acutely decompensated cirrhosis
Journal of Hepatology ( IF 26.8 ) Pub Date : 2024-10-28 , DOI: 10.1016/j.jhep.2024.10.028 Zhujun Cao, Yujing Yao, Minghao Cai, Chenxi Zhang, Yuhan Liu, Haiguang Xin, Baoyan An, Hui Wang, Yide Lu, Ziqiang Li, Yaoxing Chen, Yan Huang, Min Xin, Ruokun Li, Zhuping Qian, Yi Zhou, Xiaogang Xiang, Richard Moreau, Qing Xie
中文翻译:

1 型、2 型和 3 型炎症的血液标志物与急性失代偿期肝硬化的严重程度相关
在表现为临床明显诱因(即感染、急性肝损伤)的急性失代偿期肝硬化 (ADC) 患者中,炎症血液标志物的改变与进展为严重表型(例如,慢加急性肝衰竭、ACLF)相关。目前尚不清楚血液炎症标志物的改变是否可能与独立于诱因的 ADC 进展相关。
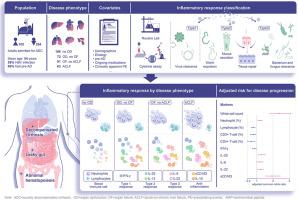
我们前瞻性地招募了 394 例因 ADC 收治的患者,这些患者被分为四种严重程度增加的表型: 无器官功能障碍 (n=168) 、仅器官功能障碍 (n=72)、无 ACLF 的器官衰竭 (n=91) 和 ACLF (n=63)。入组时获得临床血细胞计数和血清炎症标志物 (包括与 1 型、 2 型和 3 型炎症相关的可溶性标志物) 水平。使用针对混杂因素 (包括诱因) 调整的相邻类别的 logit 模型的有序回归来分析每个血液炎症标志物的变化与 ADC 恶化之间的关联。
与进展到下一个更严重阶段的较高风险相关的炎症标志物如下:中性粒细胞计数增加 (校正共同比值比 [cOR] 1.17,95% CI 1.06-1.28);2 型细胞因子白细胞介素 (IL)-25 (cOR 1.21,95%CI 1.06-1.39)、3 型细胞因子 IL-6 (cOR 1.15,95%CI 1.02-1.28) 和 IL-22 (cOR 1.16,95%CI 1.03-1.30) 或抗炎可溶性 CD163 (cOR 1.94,95%CI 1.58-2.38) 水平升高;淋巴细胞计数降低 (cOR 0.77, 95%CI 0.68-0.87) 或 1 型细胞因子 IFN-γ 水平降低 (cOR 0.85, 95%CI 0.75-0.95)。
在 ADC 患者中,与 1 型、2 型和 3 型炎症相关的细胞因子血液水平的变化,以及中性粒细胞增多、淋巴细胞减少和抗炎信号升高分别与进展为 ACLF 的风险增加相关,与临床上明显的诱因的存在无关。
更新日期:2024-10-29
Journal of Hepatology ( IF 26.8 ) Pub Date : 2024-10-28 , DOI: 10.1016/j.jhep.2024.10.028 Zhujun Cao, Yujing Yao, Minghao Cai, Chenxi Zhang, Yuhan Liu, Haiguang Xin, Baoyan An, Hui Wang, Yide Lu, Ziqiang Li, Yaoxing Chen, Yan Huang, Min Xin, Ruokun Li, Zhuping Qian, Yi Zhou, Xiaogang Xiang, Richard Moreau, Qing Xie
|
Background and aims
In patients with acutely decompensated cirrhosis (ADC) who present with clinically apparent precipitants (i.e., infections, acute liver injury), alterations in blood markers of inflammation associate with progression toward severe phenotypes (e.g., acute-on-chronic liver failure, ACLF). It is unclear whether alterations in blood inflammatory markers may associate with progression of ADC independently of precipitants.Methods
We prospectively enrolled 394 patients admitted for ADC who were classified into four phenotypes of increasing severity: no organ dysfunction (n=168), organ dysfunction alone (n=72), organ failure without ACLF (n=91), and ACLF (n=63). Clinical blood cell counts and serum levels of inflammatory markers (including soluble markers related to type-1, type-2, and type-3 inflammation) were obtained at enrollment. Ordinal regression with adjacent categories logit model adjusted for confounders (including precipitants) was used to analyze associations between changes in each blood inflammatory marker and the worsening of ADC.Results
Inflammatory markers that were associated with higher risk of progressing to the next more severe stage were as follows: increasing neutrophil counts (adjusted common odds ratio [cOR] 1.17, 95%CI 1.06-1.28); increasing levels of the type-2 cytokine interleukin (IL)-25 (cOR 1.21, 95%CI 1.06-1.39), type-3 cytokines IL-6 (cOR 1.15, 95%CI 1.02-1.28) and IL-22 (cOR 1.16, 95%CI 1.03-1.30), or anti-inflammatory soluble CD163 (cOR 1.94, 95%CI 1.58-2.38); decreasing lymphocyte counts (cOR 0.77, 95%CI 0.68-0.87), or decreasing levels of the type-1 cytokine IFN-γ (cOR 0.85, 95%CI 0.75-0.95).Conclusions
Among patients with ADC, alterations in blood levels of cytokines related to type-1, type-2 and type-3 inflammation, together with neutrophilia, lymphopenia and elevated anti-inflammatory signals were individually associated with an increased risk of progressing toward ACLF, independently of the presence of clinically apparent precipitants.中文翻译:

1 型、2 型和 3 型炎症的血液标志物与急性失代偿期肝硬化的严重程度相关
背景和目标
在表现为临床明显诱因(即感染、急性肝损伤)的急性失代偿期肝硬化 (ADC) 患者中,炎症血液标志物的改变与进展为严重表型(例如,慢加急性肝衰竭、ACLF)相关。目前尚不清楚血液炎症标志物的改变是否可能与独立于诱因的 ADC 进展相关。
方法
我们前瞻性地招募了 394 例因 ADC 收治的患者,这些患者被分为四种严重程度增加的表型: 无器官功能障碍 (n=168) 、仅器官功能障碍 (n=72)、无 ACLF 的器官衰竭 (n=91) 和 ACLF (n=63)。入组时获得临床血细胞计数和血清炎症标志物 (包括与 1 型、 2 型和 3 型炎症相关的可溶性标志物) 水平。使用针对混杂因素 (包括诱因) 调整的相邻类别的 logit 模型的有序回归来分析每个血液炎症标志物的变化与 ADC 恶化之间的关联。
结果
与进展到下一个更严重阶段的较高风险相关的炎症标志物如下:中性粒细胞计数增加 (校正共同比值比 [cOR] 1.17,95% CI 1.06-1.28);2 型细胞因子白细胞介素 (IL)-25 (cOR 1.21,95%CI 1.06-1.39)、3 型细胞因子 IL-6 (cOR 1.15,95%CI 1.02-1.28) 和 IL-22 (cOR 1.16,95%CI 1.03-1.30) 或抗炎可溶性 CD163 (cOR 1.94,95%CI 1.58-2.38) 水平升高;淋巴细胞计数降低 (cOR 0.77, 95%CI 0.68-0.87) 或 1 型细胞因子 IFN-γ 水平降低 (cOR 0.85, 95%CI 0.75-0.95)。
结论
在 ADC 患者中,与 1 型、2 型和 3 型炎症相关的细胞因子血液水平的变化,以及中性粒细胞增多、淋巴细胞减少和抗炎信号升高分别与进展为 ACLF 的风险增加相关,与临床上明显的诱因的存在无关。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号