当前位置:
X-MOL 学术
›
Aliment. Pharm. Ther.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
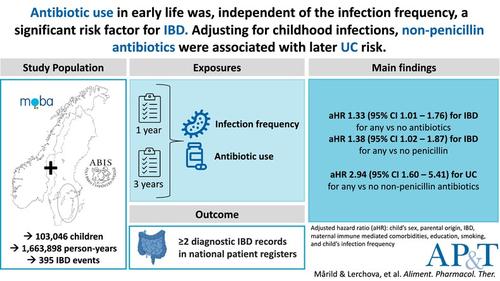
Early‐Life Infections, Antibiotics and Later Risk of Childhood and Early Adult‐Onset Inflammatory Bowel Disease: Pooled Analysis of Two Scandinavian Birth Cohorts
Alimentary Pharmacology & Therapeutics ( IF 6.6 ) Pub Date : 2024-10-25 , DOI: 10.1111/apt.18358 Karl Mårild, Tereza Lerchova, Malin Östensson, Henrik Imberg, Ketil Størdal, Johnny Ludvigsson
Alimentary Pharmacology & Therapeutics ( IF 6.6 ) Pub Date : 2024-10-25 , DOI: 10.1111/apt.18358 Karl Mårild, Tereza Lerchova, Malin Östensson, Henrik Imberg, Ketil Størdal, Johnny Ludvigsson
|
BackgroundChildhood antibiotic use has been associated with inflammatory bowel disease (IBD), although the potential contribution of infection frequency remains uncertain.AimsTo explore the association between early‐life infections, antibiotics and IBD development.MethodsWe used population‐based data from ABIS (Sweden) and MoBa (Norway) cohorts following children from birth (1997–2009) until 2021. Prospectively collected questionnaires identified infection frequency (any, gastrointestinal and respiratory) and antibiotics (any, penicillin and non‐penicillin) until age 3. IBD diagnosis required ≥ 2 records in national health registries. Cohort‐specific hazard ratios (aHR), adjusted for parental education, smoking and IBD were estimated and pooled using a random‐effects model. Antibiotic analyses were adjusted for infection frequency.ResultsThere were 103,046 children (11,872 ABIS and 91,174 MoBa), contributing to 1,663,898 person‐years of follow‐up, during which 395 were diagnosed with IBD. The frequency of any infection at 0 to < 1 and 1 to < 3 years showed a pooled aHR of 1.01 (95% confidence interval [CI] = 0.96–1.07) and 1.00 (95% CI = 0.99–1.01) per additional infection for IBD. Adjusting for infections, any versus no antibiotics in the first year was associated with IBD (pooled aHR = 1.33 [95% CI = 1.01–1.76]). The aHR for additional antibiotic course was 1.17 (95% CI = 0.96–1.44), driven by penicillin (per additional course, aHR = 1.28 [95% CI = 1.02–1.60]). Although antibiotics at 1 to < 3 years did not show an association with IBD or Crohn's disease, non‐penicillin antibiotics were associated with ulcerative colitis (per additional course, aHR = 1.95 [95% CI = 1.38–2.75]).ConclusionEarly‐life antibiotic use was, a significant risk factor for childhood and early adult‐onset IBD, independent of infection frequency.
中文翻译:

早期感染、抗生素和儿童期和成人早期发病性炎症性肠病的风险:两个斯堪的纳维亚出生队列的汇总分析
背景儿童期抗生素使用与炎症性肠病 (IBD) 有关,尽管感染频率的潜在贡献仍不确定。目的探讨早期感染、抗生素和 IBD 发展之间的关联。方法我们使用了来自 ABIS (瑞典) 和 MoBa (挪威) 队列的基于人群的数据,跟踪了从出生 (1997-2009) 到 2021 年的儿童。前瞻性收集的问卷确定了感染频率 (任何、胃肠道和呼吸系统) 和抗生素 (任何、青霉素和非青霉素) 直到 3 岁。IBD 诊断需要在国家卫生登记处≥ 2 条记录。使用随机效应模型估计和合并根据父母教育、吸烟和 IBD 调整的队列特异性风险比 (aHR)。根据感染频率调整抗生素分析。结果有 103,046 名儿童 (11,872 名 ABIS 和 91,174 名 MoBa),促成了 1,663,898 人年的随访,其中 395 人被诊断患有 IBD。3 年 0 至 < 1 和 1 至 < 的任何感染频率显示,IBD 每次额外感染的合并 aHR 为 1.01(95% 置信区间 [CI] = 0.96-1.07)和 1.00(95% CI = 0.99-1.01)。调整感染后,第一年使用抗生素与不使用抗生素与 IBD 相关(合并 aHR = 1.33 [95% CI = 1.01–1.76])。由青霉素驱动的额外抗生素疗程的 aHR 为 1.17 (95% CI = 0.96–1.44) (每个额外疗程,aHR = 1.28 [95% CI = 1.02–1.60])。尽管 3 年 1 至 < 的抗生素与 IBD 或克罗恩病无关,但非青霉素抗生素与溃疡性结肠炎有关(每个额外的疗程,aHR = 1.95 [95% CI = 1.38–2.75])。结论早期使用抗生素是儿童期和成年早期发病 IBD 的重要危险因素,与感染频率无关。
更新日期:2024-10-25
中文翻译:

早期感染、抗生素和儿童期和成人早期发病性炎症性肠病的风险:两个斯堪的纳维亚出生队列的汇总分析
背景儿童期抗生素使用与炎症性肠病 (IBD) 有关,尽管感染频率的潜在贡献仍不确定。目的探讨早期感染、抗生素和 IBD 发展之间的关联。方法我们使用了来自 ABIS (瑞典) 和 MoBa (挪威) 队列的基于人群的数据,跟踪了从出生 (1997-2009) 到 2021 年的儿童。前瞻性收集的问卷确定了感染频率 (任何、胃肠道和呼吸系统) 和抗生素 (任何、青霉素和非青霉素) 直到 3 岁。IBD 诊断需要在国家卫生登记处≥ 2 条记录。使用随机效应模型估计和合并根据父母教育、吸烟和 IBD 调整的队列特异性风险比 (aHR)。根据感染频率调整抗生素分析。结果有 103,046 名儿童 (11,872 名 ABIS 和 91,174 名 MoBa),促成了 1,663,898 人年的随访,其中 395 人被诊断患有 IBD。3 年 0 至 < 1 和 1 至 < 的任何感染频率显示,IBD 每次额外感染的合并 aHR 为 1.01(95% 置信区间 [CI] = 0.96-1.07)和 1.00(95% CI = 0.99-1.01)。调整感染后,第一年使用抗生素与不使用抗生素与 IBD 相关(合并 aHR = 1.33 [95% CI = 1.01–1.76])。由青霉素驱动的额外抗生素疗程的 aHR 为 1.17 (95% CI = 0.96–1.44) (每个额外疗程,aHR = 1.28 [95% CI = 1.02–1.60])。尽管 3 年 1 至 < 的抗生素与 IBD 或克罗恩病无关,但非青霉素抗生素与溃疡性结肠炎有关(每个额外的疗程,aHR = 1.95 [95% CI = 1.38–2.75])。结论早期使用抗生素是儿童期和成年早期发病 IBD 的重要危险因素,与感染频率无关。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号