Diabetologia ( IF 8.4 ) Pub Date : 2024-10-18 , DOI: 10.1007/s00125-024-06279-1 Stephanie Centofanti, Leonie K. Heilbronn, Gary Wittert, Jillian Dorrian, Alison M. Coates, David Kennaway, Charlotte Gupta, Jacqueline M. Stepien, Peter Catcheside, Crystal Yates, Linda Grosser, Raymond W. Matthews, Siobhan Banks
|
Aims/hypothesis
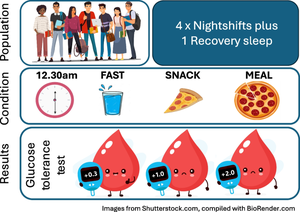
Night-shift work causes circadian misalignment and impairs glucose metabolism. We hypothesise that food intake during night shifts may contribute to this phenomenon.
Methods
This open-label, multi-arm, single-site, parallel-group controlled trial involved a 6 day stay at the University of South Australia’s sleep laboratory (Adelaide, SA, Australia). Healthy, non-shift-working adults without obesity (N=55; age 24.5 ± 4.8 years; BMI 24.8 ± 2.8 kg/m2) were assigned to the next available run date and cluster randomised (1:1:1) to fasting-at-night (N=20), snack-at-night (N=17), or meal-at-night (N=18) conditions. One participant withdrew from each group, prior to starting the study. Due to study design, neither participants nor people collecting their measurements could be blinded. Statistical and laboratory staff were concealed to study allocation. Participants were fed at calculated energy balance, with the macronutrient composition of meals being similar across conditions. The primary outcomes were a linear mixed-effects model of glucose, insulin and NEFA AUC in response to a 75 g OGTT that was conducted prior to and after 4 consecutive nights of shift work plus 1 night of recovery sleep. Insulin sensitivity, insulinogenic and disposition indexes were also calculated.
Results
Night-shift work impaired insulin sensitivity, as measured by insulin AUC (p=0.035) and the insulin sensitivity index (p=0.016) across all conditions. Insulin secretion, as measured by the insulinogenic index, was increased in the fasting-at-night condition only (p=0.030), resulting in a day×condition interaction in glucose AUC (p<0.001) such that glucose tolerance was impaired in the meal-at night (+2.00 [95% CI 1.45, 2.56], p<0.001) and snack at-night (+0.96 [0.36, 1.56], p=0.022) conditions vs the fasting-at-night (+0.34 [–0.21, 0.89]) condition. A day×condition interaction was also observed in NEFA AUC (p<0.001), being higher in the meal-at-night (+0.07 [0.03, 0.10]. p=0.001) and snack-at-night (0.01 [–0.03, 0.05], p=0.045) conditions vs the fasting-at-night condition (–0.02 [–0.06, 0.01]). No adverse events occurred.
Conclusions/interpretation
The timing of food intake has a critical effect on glucose metabolism during simulated night-shift work, which was readily amendable to a meal re-timing intervention.
Trial Registration
Australian New Zealand Clinical Trials Registry (ANZCTR) ACTRN12616001556437
Funding
This work was funded by the National Health and Medical Research Council (NHMRC), APP1099077.
Graphical Abstract
中文翻译:

禁食作为改变模拟夜班工作对健康成人葡萄糖代谢影响的干预措施:一项整群随机对照试验
目标/假设
夜班工作会导致昼夜节律错位并损害葡萄糖代谢。我们假设夜班的食物摄入可能会导致这种现象。
方法
这项开放标签、多臂、单中心、平行组对照试验涉及在南澳大利亚大学睡眠实验室(澳大利亚南澳大利亚州阿德莱德)停留 6 天。无肥胖的健康、非轮班工作的成年人 (N=55;年龄 24.5 ± 4.8 岁;BMI 24.8 ± 2.8 kg/m2) 被分配到下一个可用的运行日期,并将整群随机 (1:1:1) 分配到夜间禁食 (N=20)、夜间零食 (N=17) 或夜间进餐 (N=18) 条件。在开始研究之前,每组一名参与者退出。由于研究设计的原因,参与者和收集测量结果的人都不能被蒙法。统计和实验室工作人员被隐藏以研究分配。参与者在计算出的能量平衡下进食,不同条件下膳食的宏量营养素成分相似。主要结局是葡萄糖、胰岛素和 NEFA AUC 响应 75 g OGTT 的线性混合效应模型,该模型在连续 4 晚轮班工作加上 1 晚恢复睡眠之前和之后进行。还计算了胰岛素敏感性、胰岛素生成和处置指标。
结果
夜班工作损害了胰岛素敏感性,通过所有情况下的胰岛素 AUC (p=0.035) 和胰岛素敏感性指数 (p=0.016) 测量。通过胰岛素生成指数测量的胰岛素分泌仅在夜间禁食的情况下增加 (p=0.030),导致葡萄糖 AUC (p<0.001) ×日间相互作用,因此晚上进餐(+2.00 [95% CI 1.45, 2.56],p<0.001)和晚上吃零食(+0.96 [0.36, 1.56],p=0.022) 条件与夜间禁食 (+0.34 [–0.21, 0.89]) 条件。在 NEFA AUC (p<0.001) 中也观察到日×间条件相互作用,在夜间进餐中更高 (+0.07 [0.03, 0.10]。p=0.001) 和夜间吃零食 (0.01 [–0.03, 0.05], p=0.045) 条件与夜间禁食条件 (–0.02 [–0.06, 0.01])。未发生不良事件。
结论/解释
在模拟夜班工作期间,食物摄入的时间对葡萄糖代谢有关键影响,这很容易被修正为膳食重新定时干预。
试用注册
澳大利亚新西兰临床试验注册中心 (ANZCTR) ACTRN12616001556437
资金
这项工作由 APP1099077 年国家健康与医学研究委员会 (NHMRC) 资助。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号