Diabetologia ( IF 8.4 ) Pub Date : 2024-10-15 , DOI: 10.1007/s00125-024-06275-5 Paola S. Apaolaza, Yi-Chun Chen, Kavi Grewal, Yannik Lurz, Severin Boulassel, C. Bruce Verchere, Teresa Rodriguez-Calvo
|
Aims/hypothesis
Islet prohormone-processing enzymes convert peptide hormone precursors to mature hormones. Defective beta cell prohormone processing and the release of incompletely processed peptide hormones are observed prior to the onset of diabetes, yet molecular mechanisms underlying impaired prohormone processing during the development of diabetes remains largely unknown. Previous studies have shown that prohormone convertase 1/3 (PC1/3) protein and mRNA expression levels are reduced in whole islets from donors with type 1 diabetes, although whether PC1/3-mediated prohormone processing in alpha and beta cells is disrupted in type 1 diabetes remained to be explored. Herein, we aimed to analyse the expression of PC1/3 in islets from non-diabetic donors, autoantibody-positive donors and donors diagnosed with type 1 diabetes or type 2 diabetes.
Methods
Immunostaining and high-dimensional image analysis were performed on pancreatic sections from a cross-sectional cohort of 54 donors obtained from the Network for Pancreatic Organ Donors with Diabetes (nPOD) repository, to evaluate PC1/3 expression patterns in islet alpha, beta and delta cells at different stages of diabetes.
Results
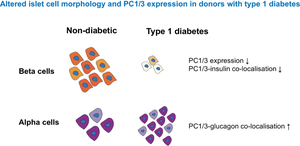
Alpha and beta cell morphology were altered in donors with type 1 diabetes, including decreased alpha and beta cell size. As expected, the insulin-positive and PC1/3-positive areas in the islets were both reduced, and this was accompanied by a reduced percentage of PC1/3-positive and insulin-positive/PC1/3-positive cells in islets. PC1/3 and insulin co-localisation was also reduced. The glucagon-positive area, as well as the percentage of glucagon-positive and glucagon-positive/PC1/3-positive cells in islets, was increased. PC1/3 and glucagon co-localisation was also increased in donors with type 1 diabetes. The somatostatin-positive cell area and somatostatin staining intensity were elevated in islets from donors with recent-onset type 1 diabetes.
Conclusions/interpretation
Our high-resolution histomorphological analysis of human pancreatic islets from donors with and without diabetes has uncovered details of the cellular origin of islet prohormone peptide processing defects. Reduced beta cell PC1/3 and increased alpha cell PC1/3 in islets from donors with type 1 diabetes pinpointed the functional deterioration of beta cells and the concomitant potential increase in PC1/3 usage for prohormone processing in alpha cells during the pathogenesis of type 1 diabetes. Our finding of PC1/3 loss in beta cells may inform the discovery of new prohormone biomarkers as indicators of beta cell dysfunction, and the finding of elevated PC1/3 expression in alpha cells may encourage the design of therapeutic targets via leveraging alpha cell adaptation in diabetes.
Graphical Abstract
中文翻译:

胰岛激素原转化酶 1/3 在糖尿病患者胰腺供体中表达的定量分析
目标/假设
胰岛激素原加工酶将肽激素前体转化为成熟激素。在糖尿病发作之前观察到 β 细胞激素原加工缺陷和未完全加工肽激素的释放,但在糖尿病发展过程中激素原加工受损的分子机制在很大程度上仍然未知。先前的研究表明,1 型糖尿病供体的整个胰岛中激素转化酶原 1/3 (PC1/3) 蛋白和 mRNA 表达水平降低,尽管 PC1/3 介导的 α 和 β 细胞中的激素原加工在 1 型糖尿病中是否被破坏仍有待探索。在此,我们旨在分析非糖尿病供体、自身抗体阳性供体和诊断为 1 型糖尿病或 2 型糖尿病的供体的胰岛中 PC1/3 的表达。
方法
对来自糖尿病胰腺器官供体网络 (nPOD) 存储库的 54 名供体横断面队列的胰腺切片进行免疫染色和高维图像分析,以评估糖尿病不同阶段胰岛 α 、 β 和 δ 细胞中 PC1/3 的表达模式。
结果
1 型糖尿病供体的 α 和 β 细胞形态发生改变,包括 α 和 β 细胞大小减小。正如预期的那样,胰岛中胰岛素阳性和 PC1/3 阳性区域均减少,这伴随着胰岛中 PC1/3 阳性和胰岛素阳性/PC1/3 阳性细胞的百分比降低。PC1/3 和胰岛素共定位也降低。胰高血糖素阳性面积以及胰高血糖素阳性和胰高血糖素阳性/PC1/3 阳性细胞的百分比增加。PC1/3 和胰高血糖素共定位在 1 型糖尿病供体中也有所增加。生长抑素阳性细胞面积和生长抑素染色强度在近期发病的 1 型糖尿病供体的胰岛中升高。
结论/解释
我们对患有糖尿病和不患有糖尿病的供体的人类胰岛进行了高分辨率组织形态学分析,揭示了胰岛激素原肽加工缺陷的细胞起源细节。1 型糖尿病供体胰岛中 β 细胞 PC1/3 减少和 α 细胞 PC1/3 增加表明 β 细胞的功能恶化以及 1 型糖尿病发病机制期间 PC1/3 用于 α 细胞激素原加工的随之而来的潜在增加。我们在 β 细胞中发现 PC1/3 缺失可能为发现新的激素原生物标志物作为 β 细胞功能障碍的指标提供信息,而 α 细胞中 PC1/3 表达升高的发现可能鼓励通过利用糖尿病中的 α 细胞适应来设计治疗靶点。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号