当前位置:
X-MOL 学术
›
Eur. J. Heart Fail.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Cardio‐ocular syndrome: Retinal microvascular changes in acutely decompensated heart failure
European Journal of Heart Failure ( IF 16.9 ) Pub Date : 2024-09-25 , DOI: 10.1002/ejhf.3474 Amr Abdin, Alaa Din Abdin, Giuseppe Merone, Wissam Aljundi, Bernhard Haring, Yaser Abu Dail, Felix Mahfoud, Insa Emrich, Hussam Al Ghorani, Elsa Wilma Böhm, Berthold Seitz, Michael Böhm
European Journal of Heart Failure ( IF 16.9 ) Pub Date : 2024-09-25 , DOI: 10.1002/ejhf.3474 Amr Abdin, Alaa Din Abdin, Giuseppe Merone, Wissam Aljundi, Bernhard Haring, Yaser Abu Dail, Felix Mahfoud, Insa Emrich, Hussam Al Ghorani, Elsa Wilma Böhm, Berthold Seitz, Michael Böhm
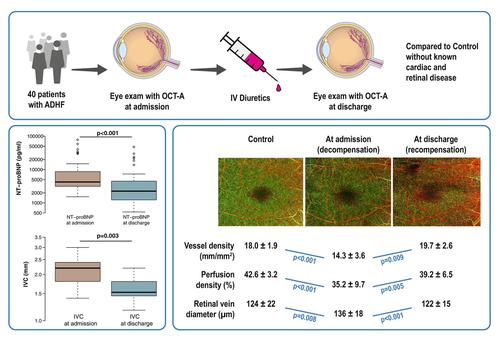
|
AimsTo investigate the changes in retinal microvasculature by contemporary imaging techniques during episodes of acute decompensated heart failure (ADHF) and following recompensation compared to age‐matched controls without known cardiac or retinal disease.Methods and resultsAdult patients hospitalized with a primary diagnosis of ADHF, regardless of left ventricular ejection fraction (LVEF) and treated with a minimum dose of 40 mg of intravenous furosemide or equivalent were included. Transthoracic echocardiography was conducted in all patients. Eye examinations were performed out within the initial 24 h after admission and after recompensation before discharge. All eyes underwent a general examination, including a best corrected visual acuity test, dilated fundoscopy, spectral‐domain optical coherence tomography (OCT) as well as OCT angiography (OCT‐A). In addition, 40 participants without documented cardiac or retinal diseases served as controls. Forty patients with ADHF (mean age 78.9 ± 8.8 years; 32% female) with a mean LVEF of 43 ± 12.8% were included. All patients were treated with intravenous diuretics for a median of 4.3 ± 2.8 days. There was a significant reduction in N‐terminal pro‐B‐type natriuretic peptide from baseline up to discharge (10 396 [interquartile range 6410] vs. 6380 [interquartile range 3933] pg/ml, p ≤ 0.001) and inferior vena cava diameters (2.13 ± 0.4 vs. 1.63 ± 0.3 cm, p = 0.003). Compared to the control group, patients with ADHF showed on admission impaired visual acuity (0.15 ± 0.1 vs. 0.35 ± 0.1 logMAR, p < 0.001), reduced macular vessel density (18.0 ± 1.9 vs. 14.3 ± 3.6 mm/mm2 , p < 0.001) and perfusion density (42.6 ± 3.2 vs. 35.2 ± 9.7%, p < 0.001). After recompensation, the mean overall vessel density and mean overall perfusion density were markedly increased at discharge (14.3 ± 3.6 vs. 19.7 ± 2.6 mm/mm2 , p = 0.001, and 35.2 ± 9.7 vs. 39.2 ± 6.5%, p = 0.005, respectively). The mean diameter of the superior temporal retinal vein at admission was significantly larger compared to the control group (136 ± 19 vs. 124 ± 22 μm, p = 0.008) and decreased significantly to 122 ± 15 μm at discharge (p < 0.001).ConclusionThis analysis revealed a remarkable reversible change in retinal microvasculature after ADHF. This could provide a valuable evidence for use of OCT‐A in the assessment of overall microperfusion and haemodynamic status in patients with acute heart failure.
中文翻译:

心眼综合征:急性失代偿性心力衰竭的视网膜微血管变化
目的 通过当代成像技术研究急性失代偿性心力衰竭 (ADHF) 发作期间和再代偿后与没有已知心脏或视网膜疾病的年龄匹配对照相比视网膜微血管的变化。方法和结果初步诊断为 ADHF 住院的成年患者,无论情况如何包括左心室射血分数 (LVEF) 和最小剂量 40 mg 静脉注射呋塞米或等效药物治疗。对所有患者进行经胸超声心动图检查。入院后最初 24 小时内以及出院前再代偿后进行眼部检查。所有眼睛均接受一般检查,包括最佳矫正视力测试、散瞳眼底镜检查、谱域光学相干断层扫描(OCT)以及OCT血管造影(OCT-A)。此外,40 名没有心脏病或视网膜疾病记录的参与者作为对照。包括 40 名 ADHF 患者(平均年龄 78.9 ± 8.8 岁;32% 为女性),平均 LVEF 为 43 ± 12.8%。所有患者均接受静脉利尿剂治疗,中位治疗时间为 4.3 ± 2.8 天。从基线到出院,N 末端 B 型利钠肽前体显着减少(10 396 [四分位距 6410] 与 6380 [四分位距 3933] pg/ml,p ≤ 0.001)和下腔静脉直径显着减少(2.13 ± 0.4 与 1.63 ± 0.3 厘米,p = 0.003)。与对照组相比,ADHF 患者入院时表现出视力受损(0.15 ± 0.1 vs. 0.35 ± 0.1 logMAR,p < 0.001),黄斑血管密度降低(18.0 ± 1.9 vs. 14.3 ± 3.6 mm/mm2,p < 0.001)和灌注密度(42.6 ± 3.2 vs. 35.2 ± 9.7%,p < 0.001)。 再补偿后,出院时平均总血管密度和平均总灌注密度显着增加(14.3 ± 3.6 vs. 19.7 ± 2.6 mm/mm2,p = 0.001,35.2 ± 9.7 vs. 39.2 ± 6.5%,p = 0.005,分别)。入院时视网膜上静脉的平均直径显着大于对照组(136 ± 19 vs. 124 ± 22 μm,p = 0.008),出院时显着下降至 122 ± 15 μm(p < 0.001)结论该分析揭示了 ADHF 后视网膜微血管系统发生显着的可逆变化。这可以为使用OCT-A评估急性心力衰竭患者的整体微灌注和血流动力学状态提供有价值的证据。
更新日期:2024-09-25
中文翻译:

心眼综合征:急性失代偿性心力衰竭的视网膜微血管变化
目的 通过当代成像技术研究急性失代偿性心力衰竭 (ADHF) 发作期间和再代偿后与没有已知心脏或视网膜疾病的年龄匹配对照相比视网膜微血管的变化。方法和结果初步诊断为 ADHF 住院的成年患者,无论情况如何包括左心室射血分数 (LVEF) 和最小剂量 40 mg 静脉注射呋塞米或等效药物治疗。对所有患者进行经胸超声心动图检查。入院后最初 24 小时内以及出院前再代偿后进行眼部检查。所有眼睛均接受一般检查,包括最佳矫正视力测试、散瞳眼底镜检查、谱域光学相干断层扫描(OCT)以及OCT血管造影(OCT-A)。此外,40 名没有心脏病或视网膜疾病记录的参与者作为对照。包括 40 名 ADHF 患者(平均年龄 78.9 ± 8.8 岁;32% 为女性),平均 LVEF 为 43 ± 12.8%。所有患者均接受静脉利尿剂治疗,中位治疗时间为 4.3 ± 2.8 天。从基线到出院,N 末端 B 型利钠肽前体显着减少(10 396 [四分位距 6410] 与 6380 [四分位距 3933] pg/ml,p ≤ 0.001)和下腔静脉直径显着减少(2.13 ± 0.4 与 1.63 ± 0.3 厘米,p = 0.003)。与对照组相比,ADHF 患者入院时表现出视力受损(0.15 ± 0.1 vs. 0.35 ± 0.1 logMAR,p < 0.001),黄斑血管密度降低(18.0 ± 1.9 vs. 14.3 ± 3.6 mm/mm2,p < 0.001)和灌注密度(42.6 ± 3.2 vs. 35.2 ± 9.7%,p < 0.001)。 再补偿后,出院时平均总血管密度和平均总灌注密度显着增加(14.3 ± 3.6 vs. 19.7 ± 2.6 mm/mm2,p = 0.001,35.2 ± 9.7 vs. 39.2 ± 6.5%,p = 0.005,分别)。入院时视网膜上静脉的平均直径显着大于对照组(136 ± 19 vs. 124 ± 22 μm,p = 0.008),出院时显着下降至 122 ± 15 μm(p < 0.001)结论该分析揭示了 ADHF 后视网膜微血管系统发生显着的可逆变化。这可以为使用OCT-A评估急性心力衰竭患者的整体微灌注和血流动力学状态提供有价值的证据。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号