当前位置:
X-MOL 学术
›
J. Adv. Res.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Dialog between mantle cell lymphoma cells and lymphoma-associated macrophages underlies ibrutinib resistance
Journal of Advanced Research ( IF 11.4 ) Pub Date : 2024-08-19 , DOI: 10.1016/j.jare.2024.08.023 Xiaoqing Sun 1 , Caiqin Wang 2 , Jianghua Cao 3 , Jing Li 3 , Gang Ma 1 , Xianqiu Wu 4 , Peng Sun 3 , Yu Wang 3 , Jiajia Huang 3 , Robert Peter Gale 5 , Zhiming Li 3
中文翻译:

套细胞淋巴瘤细胞与淋巴瘤相关巨噬细胞之间的对话是依鲁替尼耐药的基础
套细胞淋巴瘤 (MCL) 患者经常对依鲁替尼产生耐药性。淋巴瘤相关巨噬细胞 (LAM) 可能在这种耐药性中起因果作用,但在目前的文献中仍未得到充分探索。
阐明 LAMs 在介导 MCL 中依鲁替尼耐药的作用。
我们通过多参数流式细胞术 (MPFC) 使用对伊布替尼耐药和敏感的 MCL 患者血液和组织样本中的 CD206 和 CD86 抗体研究了巨噬细胞极化。随后,我们开发了一种利用 MCL 细胞系的体外共培养模型来识别与依鲁替尼耐药和巨噬细胞 M2 极化相关的细胞因子。使用 MPFC 、 RNA 测序和 Western blot 分析检查耐药的潜在机制。此外,我们还评估了 SB225002(一种 CXCR2 抑制剂)是否可以通过 CCK-8 和 caspase-3 测定以及在涉及伊布替尼耐药 MCL 细胞系的小鼠异种移植模型中逆转依鲁替尼耐药。
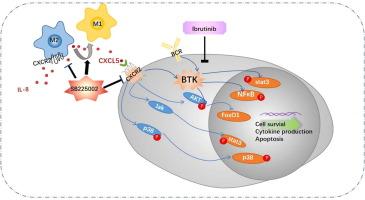
在表现出伊布替尼耐药的患者中,与敏感患者相比,M2 与 M1 LAMs 的比率显着升高。在 LAMs 和 MCL 细胞的共培养中,M2 巨噬细胞的百分比、依鲁替尼的 IC50 值以及 IL-8 和 CXCL5 的浓度显著升高。从机制上讲,LAM 分泌的 CXCL5 与 MCL 细胞上的 CXCR2 相互作用,导致在依鲁替尼存在下激活 Akt、p38 和 STAT3 信号通路;这种活性在 CXCL5/CXCR2 轴被阻断后减弱。与单独使用伊布替尼治疗相比,SB225002 和伊布替尼的组合显着增强了 MCL 细胞凋亡,抑制了异种移植模型中的淋巴瘤生长,并重编程了巨噬细胞表型。
我们的数据表明,在 MCL 模型中,M2 极化 LAMs 与依鲁替尼耐药性相关,并且 CXCR2 抑制剂可以逆转这种耐药性。这些发现表明了一种潜在的新治疗策略。
更新日期:2024-08-19
Journal of Advanced Research ( IF 11.4 ) Pub Date : 2024-08-19 , DOI: 10.1016/j.jare.2024.08.023 Xiaoqing Sun 1 , Caiqin Wang 2 , Jianghua Cao 3 , Jing Li 3 , Gang Ma 1 , Xianqiu Wu 4 , Peng Sun 3 , Yu Wang 3 , Jiajia Huang 3 , Robert Peter Gale 5 , Zhiming Li 3
Affiliation
|
Introduction
Patients with mantle cell lymphoma (MCL) frequently develop resistance to ibrutinib. Lymphoma-associated macrophages (LAMs) may play a causal role in this resistance but remain underexplored in current literature.Objectives
To elucidate the role of LAMs in mediating ibrutinib resistance in MCL.Methods
We investigated macrophage polarization through multiparameter flow cytometry (MPFC) using antibodies against CD206 and CD86 in blood and tissue samples from patients with MCL, both resistant and sensitive to ibrutinib. Subsequently, we developed an in vitro co-culture model utilizing MCL cell lines to identify cytokines associated with ibrutinib resistance and macrophage M2 polarization. The mechanisms underlying resistance were examined using MPFC, RNA sequencing, and Western blot analysis. Additionally, we assessed whether SB225002, a CXCR2 inhibitor, could reverse ibrutinib resistance through CCK-8 and caspase-3 assays, as well as in a mouse xenograft model involving an ibrutinib-resistant MCL cell line.Results
In patients exhibiting ibrutinib resistance, the ratio of M2 to M1 LAMs was significantly higher compared to sensitive patients. In co-cultures of LAMs and MCL cells, the percentage of M2 macrophages, the IC50 value for ibrutinib, and the concentrations of IL-8 and CXCL5 were significantly elevated. Mechanistically, CXCL5 secreted by LAMs interacted with the CXCR2 on MCL cells, leading to the activation of the Akt, p38, and STAT3 signaling pathways in the presence of ibrutinib; this activity was diminished upon blockade of the CXCL5/CXCR2 axis. The combination of SB225002 and ibrutinib significantly enhanced MCL cell apoptosis, suppressed lymphoma growth in the xenograft model, and reprogrammed macrophage phenotype compared to treatment with ibrutinib alone.Conclusion
Our data indicate that M2-polarized LAMs are associated with ibrutinib resistance in a model of MCL, and that a CXCR2 inhibitor can reverse this resistance. These findings suggest a potential new therapeutic strategy.中文翻译:

套细胞淋巴瘤细胞与淋巴瘤相关巨噬细胞之间的对话是依鲁替尼耐药的基础
介绍
套细胞淋巴瘤 (MCL) 患者经常对依鲁替尼产生耐药性。淋巴瘤相关巨噬细胞 (LAM) 可能在这种耐药性中起因果作用,但在目前的文献中仍未得到充分探索。
目标
阐明 LAMs 在介导 MCL 中依鲁替尼耐药的作用。
方法
我们通过多参数流式细胞术 (MPFC) 使用对伊布替尼耐药和敏感的 MCL 患者血液和组织样本中的 CD206 和 CD86 抗体研究了巨噬细胞极化。随后,我们开发了一种利用 MCL 细胞系的体外共培养模型来识别与依鲁替尼耐药和巨噬细胞 M2 极化相关的细胞因子。使用 MPFC 、 RNA 测序和 Western blot 分析检查耐药的潜在机制。此外,我们还评估了 SB225002(一种 CXCR2 抑制剂)是否可以通过 CCK-8 和 caspase-3 测定以及在涉及伊布替尼耐药 MCL 细胞系的小鼠异种移植模型中逆转依鲁替尼耐药。
结果
在表现出伊布替尼耐药的患者中,与敏感患者相比,M2 与 M1 LAMs 的比率显着升高。在 LAMs 和 MCL 细胞的共培养中,M2 巨噬细胞的百分比、依鲁替尼的 IC50 值以及 IL-8 和 CXCL5 的浓度显著升高。从机制上讲,LAM 分泌的 CXCL5 与 MCL 细胞上的 CXCR2 相互作用,导致在依鲁替尼存在下激活 Akt、p38 和 STAT3 信号通路;这种活性在 CXCL5/CXCR2 轴被阻断后减弱。与单独使用伊布替尼治疗相比,SB225002 和伊布替尼的组合显着增强了 MCL 细胞凋亡,抑制了异种移植模型中的淋巴瘤生长,并重编程了巨噬细胞表型。
结论
我们的数据表明,在 MCL 模型中,M2 极化 LAMs 与依鲁替尼耐药性相关,并且 CXCR2 抑制剂可以逆转这种耐药性。这些发现表明了一种潜在的新治疗策略。

































 京公网安备 11010802027423号
京公网安备 11010802027423号