Diabetologia ( IF 8.4 ) Pub Date : 2024-07-10 , DOI: 10.1007/s00125-024-06219-z Clara Luna-Marco 1, 2 , Deédeni Devos 1 , Julia Cacace 1 , Meylin Fernandez-Reyes 1 , Pedro Díaz-Pozo 1 , Juan D Salazar 1 , Eva Solá 1 , Carlos Morillas 1 , Milagros Rocha 1, 3 , Víctor M Víctor 1, 2, 3 , Susana Rovira-Llopis 1, 2
|
Aims/hypothesis
Alterations in circadian rhythms increase the likelihood of developing type 2 diabetes and CVD. Circadian rhythms are controlled by several core clock genes, which are expressed in nearly every cell, including immune cells. Immune cells are key players in the pathophysiology of type 2 diabetes, and participate in the atherosclerotic process that underlies cardiovascular risk in these patients. The role of the core clock in the leukocytes of people with type 2 diabetes and the inflammatory process associated with it are unknown. We aimed to evaluate whether the molecular clock system is impaired in the leukocytes of type 2 diabetes patients and to explore the mechanism by which this alteration leads to an increased cardiovascular risk in this population.
Methods
This is an observational cross-sectional study performed in 25 participants with type 2 diabetes and 28 healthy control participants. Clinical and biochemical parameters were obtained. Peripheral blood leukocytes were isolated using magnetic bead technology. RNA and protein lysates were obtained to assess clock-related gene transcript and protein levels using real-time PCR and western blot, respectively. Luminex XMAP technology was used to assess levels of inflammatory markers. Leukocyte–endothelial interaction assays were performed by perfusing participants’ leukocytes or THP-1 cells (with/without CLK8) over a HUVEC monolayer in a parallel flow chamber using a dynamic adhesion system.
Results
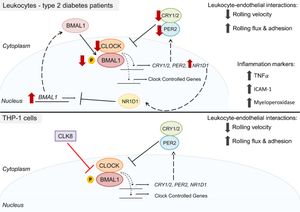
Participants with type 2 diabetes showed increased BMAL1 and NR1D1 mRNA levels and decreased protein levels of circadian locomotor output cycles kaput (CLOCK), cryptochrome 1 (CRY1), phosphorylated basic helix-loop-helix ARNT like 1 (p-BMAL1) and period circadian protein homologue 2 (PER2). Correlation studies revealed that these alterations in clock proteins were negatively associated with glucose, HbA1c, insulin and HOMA-IR levels and leukocyte cell counts. The leukocyte rolling velocity was reduced and rolling flux and adhesion were enhanced in individuals with type 2 diabetes compared with healthy participants. Interestingly, inhibition of CLOCK/BMAL1 activity in leukocytes using the CLOCK inhibitor CLK8 mimicked the effects of type 2 diabetes on leukocyte–endothelial interactions.
Conclusions/interpretation
Our study demonstrates alterations in the molecular clock system in leukocytes of individuals with type 2 diabetes, manifested in increased mRNA levels and decreased protein levels of the core clock machinery. These alterations correlated with the impaired metabolic and proinflammatory profile of the participants with type 2 diabetes. Our findings support a causal role for decreased CLOCK/BMAL1 activity in the increased level of leukocyte–endothelial interactions. Overall, our data suggest that alterations in core clock proteins accelerate the inflammatory process, which may ultimately precipitate the onset of CVD in patients with type 2 diabetes.
Graphical Abstract
中文翻译:

2 型糖尿病和超重患者白细胞的分子生物钟紊乱及其与白细胞-内皮相互作用的关系
目标/假设
昼夜节律的改变会增加患 2 型糖尿病和 CVD 的可能性。昼夜节律由几个核心时钟基因控制,这些基因几乎在每个细胞中表达,包括免疫细胞。免疫细胞是 2 型糖尿病病理生理学的关键参与者,并参与导致这些患者心血管风险的动脉粥样硬化过程。核心时钟在 2 型糖尿病患者白细胞中的作用以及与之相关的炎症过程尚不清楚。我们的目的是评估 2 型糖尿病患者白细胞中的分子时钟系统是否受损,并探讨这种改变导致该人群心血管风险增加的机制。
方法
这是一项对 25 名 2 型糖尿病患者和 28 名健康对照参与者进行的观察性横断面研究。获得临床和生化参数。使用磁珠技术分离外周血白细胞。获得 RNA 和蛋白质裂解物,分别使用实时 PCR 和蛋白质印迹评估时钟相关基因转录物和蛋白质水平。 Luminex XMAP 技术用于评估炎症标志物的水平。白细胞-内皮相互作用测定是通过使用动态粘附系统在平行流动室中的 HUVEC 单层上灌注参与者的白细胞或 THP-1 细胞(有/没有 CLK8)来进行的。
结果
2 型糖尿病参与者的BMAL1和NR1D1 mRNA 水平升高,昼夜运动输出周期 kaput (CLOCK)、隐花色素 1 (CRY1)、磷酸化碱性螺旋-环-螺旋 ARNT 样 1 (p-BMAL1) 和周期昼夜节律的蛋白质水平降低蛋白质同源物 2 (PER2)。相关性研究表明,时钟蛋白的这些变化与葡萄糖、HbA 1c 、胰岛素和 HOMA-IR 水平以及白细胞计数呈负相关。与健康参与者相比,2 型糖尿病患者的白细胞滚动速度降低,滚动通量和粘附增强。有趣的是,使用 CLOCK 抑制剂 CLK8 抑制白细胞中的 CLOCK/BMAL1 活性,模拟了 2 型糖尿病对白细胞-内皮相互作用的影响。
结论/解释
我们的研究表明,2 型糖尿病患者的白细胞分子时钟系统发生了变化,表现为核心时钟机制的 mRNA 水平增加和蛋白质水平降低。这些改变与 2 型糖尿病参与者代谢和促炎特征受损相关。我们的研究结果支持 CLOCK/BMAL1 活性降低与白细胞-内皮相互作用水平增加之间的因果关系。总体而言,我们的数据表明,核心时钟蛋白的改变加速了炎症过程,这可能最终促使 2 型糖尿病患者发生 CVD。
















































 京公网安备 11010802027423号
京公网安备 11010802027423号