当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
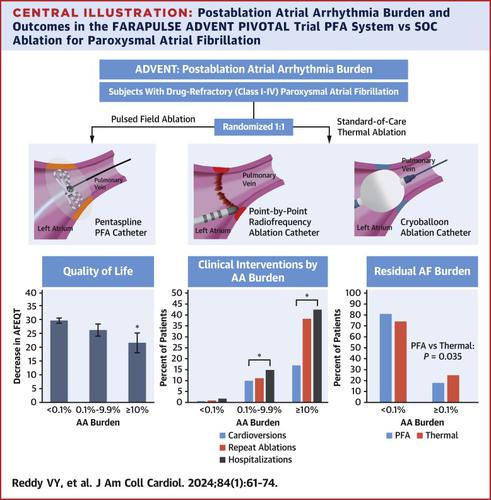
Pulsed Field vs Conventional Thermal Ablation for Paroxysmal Atrial Fibrillation: Recurrent Atrial Arrhythmia Burden
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2024-05-18 , DOI: 10.1016/j.jacc.2024.05.001 Vivek Y Reddy 1 , Moussa Mansour 2 , Hugh Calkins 3 , Andre d'Avila 4 , Larry Chinitz 5 , Christopher Woods 6 , Sanjaya K Gupta 7 , Jamie Kim 8 , Zayd A Eldadah 9 , Robert A Pickett 10 , Jeffrey Winterfield 11 , Wilber W Su 12 , Jonathan W Waks 4 , Christopher W Schneider 13 , Elizabeth Richards 13 , Elizabeth M Albrecht 13 , Brad S Sutton 13 , Edward P Gerstenfeld 14 ,
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2024-05-18 , DOI: 10.1016/j.jacc.2024.05.001 Vivek Y Reddy 1 , Moussa Mansour 2 , Hugh Calkins 3 , Andre d'Avila 4 , Larry Chinitz 5 , Christopher Woods 6 , Sanjaya K Gupta 7 , Jamie Kim 8 , Zayd A Eldadah 9 , Robert A Pickett 10 , Jeffrey Winterfield 11 , Wilber W Su 12 , Jonathan W Waks 4 , Christopher W Schneider 13 , Elizabeth Richards 13 , Elizabeth M Albrecht 13 , Brad S Sutton 13 , Edward P Gerstenfeld 14 ,
Affiliation
|
The ADVENT randomized trial revealed no significant difference in 1-year freedom from atrial arrhythmias (AA) between thermal (radiofrequency/cryoballoon) and pulsed field ablation (PFA). However, recent studies indicate that the postablation AA burden is a better predictor of clinical outcomes than the dichotomous endpoint of 30-second AA recurrence. The goal of this study was to determine: 1) the impact of postablation AA burden on outcomes; and 2) the effect of ablation modality on AA burden. In ADVENT, symptomatic drug-refractory patients with paroxysmal atrial fibrillation underwent PFA or thermal ablation. Postablation transtelephonic electrocardiogram monitor recordings were collected weekly or for symptoms, and 72-hour Holters were at 6 and 12 months. AA burden was calculated from percentage AA on Holters and transtelephonic electrocardiogram monitors. Quality-of-life assessments were at baseline and 12 months. From 593 randomized patients (299 PFA, 294 thermal), using aggregate PFA/thermal data, an AA burden exceeding 0.1% was associated with a significantly reduced quality of life and an increase in clinical interventions: redo ablation, cardioversion, and hospitalization. There were more patients with residual AA burden <0.1% with PFA than thermal ablation (OR: 1.5; 95% CI: 1.0-2.3; = 0.04). Evaluation of outcomes by baseline demographics revealed that patients with prior failed class I/III antiarrhythmic drugs had less residual AA burden after PFA compared to thermal ablation (OR: 2.5; 95% CI: 1.4-4.3; = 0.002); patients receiving only class II/IV antiarrhythmic drugs pre-ablation had no difference in AA burden between ablation groups. Compared with thermal ablation, PFA more often resulted in an AA burden less than the clinically significant threshold of 0.1% burden. (The FARAPULSE ADVENT PIVOTAL Trial PFA System vs SOC Ablation for Paroxysmal Atrial Fibrillation [ADVENT]; )
中文翻译:

脉冲场与传统热消融治疗阵发性心房颤动:复发性房性心律失常的负担
ADVENT 随机试验显示,热消融(射频/冷冻球囊)和脉冲场消融 (PFA) 之间 1 年无房性心律失常 (AA) 的情况没有显着差异。然而,最近的研究表明,消融后 AA 负担比 30 秒 AA 复发的二分终点更能预测临床结果。本研究的目的是确定:1)消融后 AA 负担对结果的影响; 2) 消融方式对 AA 负担的影响。在 ADVENT 中,有症状的药物难治性阵发性房颤患者接受了 PFA 或热消融。每周收集消融后电话心电图监测记录或收集症状,并在 6 个月和 12 个月时进行 72 小时动态心电图监测。 AA 负担是根据动态心电图和电话心电图监测仪上的 AA 百分比计算的。生活质量评估是在基线和 12 个月时进行的。从 593 名随机患者(299 名 PFA,294 名热患者)中,使用汇总的 PFA/热数据发现,AA 负担超过 0.1% 与生活质量显着下降和临床干预措施(重做消融、心脏复律和住院治疗)的增加相关。与热消融相比,PFA 治疗后残留 AA 负担 <0.1% 的患者更多(OR:1.5;95% CI:1.0-2.3;= 0.04)。通过基线人口统计学对结果进行的评估显示,与热消融相比,既往使用 I/III 类抗心律失常药物失败的患者在 PFA 后残余 AA 负担较少(OR:2.5;95% CI:1.4-4.3;= 0.002);消融前仅接受 II/IV 类抗心律失常药物的患者在消融组之间的 AA 负荷没有差异。 与热消融相比,PFA 更常导致 AA 负荷低于 0.1% 负荷的临床显着阈值。(FARAPULSE ADVENT PIVOTAL 试验 PFA 系统与 SOC 消融治疗阵发性心房颤动 [ADVENT];)
更新日期:2024-05-18
中文翻译:

脉冲场与传统热消融治疗阵发性心房颤动:复发性房性心律失常的负担
ADVENT 随机试验显示,热消融(射频/冷冻球囊)和脉冲场消融 (PFA) 之间 1 年无房性心律失常 (AA) 的情况没有显着差异。然而,最近的研究表明,消融后 AA 负担比 30 秒 AA 复发的二分终点更能预测临床结果。本研究的目的是确定:1)消融后 AA 负担对结果的影响; 2) 消融方式对 AA 负担的影响。在 ADVENT 中,有症状的药物难治性阵发性房颤患者接受了 PFA 或热消融。每周收集消融后电话心电图监测记录或收集症状,并在 6 个月和 12 个月时进行 72 小时动态心电图监测。 AA 负担是根据动态心电图和电话心电图监测仪上的 AA 百分比计算的。生活质量评估是在基线和 12 个月时进行的。从 593 名随机患者(299 名 PFA,294 名热患者)中,使用汇总的 PFA/热数据发现,AA 负担超过 0.1% 与生活质量显着下降和临床干预措施(重做消融、心脏复律和住院治疗)的增加相关。与热消融相比,PFA 治疗后残留 AA 负担 <0.1% 的患者更多(OR:1.5;95% CI:1.0-2.3;= 0.04)。通过基线人口统计学对结果进行的评估显示,与热消融相比,既往使用 I/III 类抗心律失常药物失败的患者在 PFA 后残余 AA 负担较少(OR:2.5;95% CI:1.4-4.3;= 0.002);消融前仅接受 II/IV 类抗心律失常药物的患者在消融组之间的 AA 负荷没有差异。 与热消融相比,PFA 更常导致 AA 负荷低于 0.1% 负荷的临床显着阈值。(FARAPULSE ADVENT PIVOTAL 试验 PFA 系统与 SOC 消融治疗阵发性心房颤动 [ADVENT];)































 京公网安备 11010802027423号
京公网安备 11010802027423号