CardioVascular and Interventional Radiology ( IF 2.8 ) Pub Date : 2024-06-10 , DOI: 10.1007/s00270-024-03778-x Ali Husnain 1 , Asad Malik 1 , Juan Caicedo 2 , Satish Nadig 2 , Daniel Borja-Cacho 2 , Justin Boike 3 , Josh Levitsky 3 , Allison Reiland 1 , Bartley Thornburg 1 , Rajesh Keswani 3 , Muhammed Sufyaan Ebrahim Patel 1 , Aziz Aadam 3 , Riad Salem 1 , Andres Duarte 3 , Daniel Ganger 3 , Ahsun Riaz 1
|
Purpose
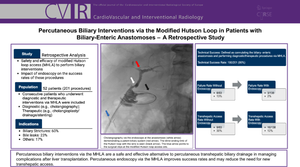
This study aimed to present the institutional experience and algorithm for performing biliary interventions in liver transplant patients using the modified Hutson loop access (MHLA) and the impact of percutaneous endoscopy via the MHLA on these procedures.
Methods
Over 13 years, 201 MHLA procedures were attempted on 52 patients (45 liver transplants; 24 living and 21 deceased donors) for diagnostic (e.g., cholangiography) and therapeutic (e.g., stent/drain insertion and cholangioplasty) purposes. The most common indications for MHLA were biliary strictures (60%) and bile leaks (23%). Percutaneous endoscopy was used to directly visualize the biliary-enteric anastomosis, diagnose pathology (e.g., ischemic cholangiopathy), and help in biliary hygiene (removing debris/casts/stones/stents) in 138/201 (69%) procedures. Technical success was defined as cannulating the biliary-enteric anastomosis and performing diagnostic/therapeutic procedure via the MHLA.
Results
The technical success rate was 95% (190/201). The failure rate among procedures performed with and without endoscopy was 2% (3/138) versus 13% (8/63) (P = 0.0024), and the need for new transhepatic access (to aid the procedure) was 12% (16/138) versus 30% (19/63) (P = 0.001). Despite endoscopy, failure in 2% of the cases resulted from inflamed/friable anastomosis (1/3) and high-grade stricture (2/3) obstructing retrograde cannulation of biliary-enteric anastomosis. Major adverse events (bowel perforation and injury) occurred in 1% of the procedures, with no procedure-related mortality.
Conclusions
MHLA-based percutaneous biliary intervention is a safe and effective alternative to managing complications after liver transplant. Percutaneous endoscopy via the MHLA improves success rates and may reduce the need for new transhepatic access.
Level of Evidence Level 4
Graphical Abstract
中文翻译:

通过改良 Hutson 环进行经皮胆道干预治疗胆肠吻合术患者:一项回顾性研究
目的
本研究旨在介绍使用改良 Hutson 环路 (MHLA) 对肝移植患者进行胆道干预的机构经验和算法,以及通过 MHLA 进行经皮内窥镜检查对这些手术的影响。
方法
13 年来,为了诊断(例如胆管造影)和治疗(例如支架/引流管插入和胆管成形术)目的,对 52 名患者(45 例肝移植;24 名活体捐献者和 21 名已故捐献者)尝试了 201 次 MHLA 手术。 MHLA 最常见的适应症是胆管狭窄 (60%) 和胆漏 (23%)。在 138/201 (69%) 的手术中,经皮内窥镜用于直接观察胆肠吻合、诊断病理学(例如缺血性胆管病)并帮助胆道卫生(清除碎片/管型/结石/支架)。技术成功被定义为胆肠吻合术插管并通过 MHLA 执行诊断/治疗程序。
结果
技术成功率为95%(190/201)。使用和不使用内窥镜检查进行的手术的失败率分别为 2% (3/138) 和 13% (8/63) ( P = 0.0024),并且需要新的肝穿刺通路(以辅助手术)为 12% (16 /138) 与 30% (19/63) ( P = 0.001)。尽管进行了内窥镜检查,仍有 2% 的病例因吻合口发炎/易碎 (1/3) 和胆肠吻合术逆行插管阻塞的高度狭窄 (2/3) 导致失败。 1% 的手术发生主要不良事件(肠穿孔和损伤),没有与手术相关的死亡。
结论
基于 MHLA 的经皮胆道介入治疗是治疗肝移植后并发症的安全有效的替代方案。通过 MHLA 进行经皮内窥镜检查可提高成功率,并可能减少新的肝穿刺通路的需求。
证据级别4 级































 京公网安备 11010802027423号
京公网安备 11010802027423号