Diabetologia ( IF 8.4 ) Pub Date : 2024-05-21 , DOI: 10.1007/s00125-024-06169-6 Danielle E Haslam 1, 2 , Liming Liang 3, 4 , Kai Guo 5 , Marijulie Martínez-Lozano 5 , Cynthia M Pérez 6 , Chih-Hao Lee 7 , Evangelia Morou-Bermudez 8 , Clary Clish 9 , David T W Wong 10 , JoAnn E Manson 1, 3, 11 , Frank B Hu 1, 2, 3 , Meir J Stampfer 1, 2, 3 , Kaumudi Joshipura 3, 5 , Shilpa N Bhupathiraju 1, 2
|
Aims/hypothesis
Many studies have examined the relationship between plasma metabolites and type 2 diabetes progression, but few have explored saliva and multi-fluid metabolites.
Methods
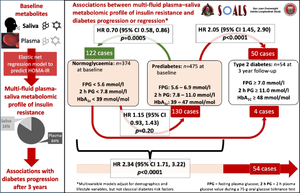
We used LC/MS to measure plasma (n=1051) and saliva (n=635) metabolites among Puerto Rican adults from the San Juan Overweight Adults Longitudinal Study. We used elastic net regression to identify plasma, saliva and multi-fluid plasma–saliva metabolomic scores predicting baseline HOMA-IR in a training set (n=509) and validated these scores in a testing set (n=340). We used multivariable Cox proportional hazards models to estimate HRs for the association of baseline metabolomic scores predicting insulin resistance with incident type 2 diabetes (n=54) and prediabetes (characterised by impaired glucose tolerance, impaired fasting glucose and/or high HbA1c) (n=130) at 3 years, along with regression from prediabetes to normoglycaemia (n=122), adjusting for traditional diabetes-related risk factors.
Results
Plasma, saliva and multi-fluid plasma–saliva metabolomic scores predicting insulin resistance included highly weighted metabolites from fructose, tyrosine, lipid and amino acid metabolism. Each SD increase in the plasma (HR 1.99 [95% CI 1.18, 3.38]; p=0.01) and multi-fluid (1.80 [1.06, 3.07]; p=0.03) metabolomic scores was associated with higher risk of type 2 diabetes. The saliva metabolomic score was associated with incident prediabetes (1.48 [1.17, 1.86]; p=0.001). All three metabolomic scores were significantly associated with lower likelihood of regressing from prediabetes to normoglycaemia in models adjusting for adiposity (HRs 0.72 for plasma, 0.78 for saliva and 0.72 for multi-fluid), but associations were attenuated when adjusting for lipid and glycaemic measures.
Conclusions/interpretation
The plasma metabolomic score predicting insulin resistance was more strongly associated with incident type 2 diabetes than the saliva metabolomic score. Only the saliva metabolomic score was associated with incident prediabetes.
Graphical Abstract
中文翻译:

发现和验证血浆、唾液和多液体血浆-唾液代谢组学评分,预测波多黎各成年人胰岛素抵抗和糖尿病进展或消退
目标/假设
许多研究检查了血浆代谢物与 2 型糖尿病进展之间的关系,但很少有研究探讨唾液和多液体代谢物。
方法
我们使用 LC/MS 测量了圣胡安超重成人纵向研究中波多黎各成人的血浆 (n=1051) 和唾液 (n=635) 代谢物。我们使用弹性网回归来识别血浆、唾液和多流体血浆-唾液代谢组学评分,预测训练集中的基线 HOMA-IR (n=509),并在测试集中验证这些评分 (n=340)。我们使用多变量 Cox 比例风险模型来估计预测胰岛素抵抗的基线代谢组学评分与 2 型糖尿病 (n=54) 和糖尿病前期 (特征为葡萄糖耐量受损、空腹血糖受损和/或 HbA1c 高) (n=130) 的相关性,以及从糖尿病前期到正常血糖的消退 (n=122), 调整传统的糖尿病相关风险因素。
结果
预测胰岛素抵抗的血浆、唾液和多液体血浆-唾液代谢组学评分包括来自果糖、酪氨酸、脂质和氨基酸代谢的高加权代谢物。血浆中每增加一个 SD (HR 1.99 [95% CI 1.18, 3.38];p=0.01)和多流体 (1.80 [1.06, 3.07];p=0.03) 代谢组学评分与 2 型糖尿病风险较高相关。唾液代谢组学评分与糖尿病前期事件相关 (1.48 [1.17, 1.86];p = 0.001)。在调整肥胖的模型中,所有三个代谢组学评分都与从糖尿病前期消退到正常血糖的较低可能性显著相关 (血浆 HRs 为 0.72,唾液为 0.78,多液体为 0.72),但在调整脂质和血糖指标时,相关性减弱。
结论/解释
预测胰岛素抵抗的血浆代谢组学评分比唾液代谢组学评分与 2 型糖尿病的发病率更强相关。只有唾液代谢组学评分与糖尿病前期事件相关。
















































 京公网安备 11010802027423号
京公网安备 11010802027423号