当前位置:
X-MOL 学术
›
JACC Heart Fail.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Factors Impacting Physician Prognostic Accuracy in Heart Failure Patients With Reduced Left Ventricular Ejection Fraction
JACC: Heart Failure ( IF 10.3 ) Pub Date : 2024-03-27 , DOI: 10.1016/j.jchf.2024.02.009 Ana C Alba 1 , Tayler A Buchan 1 , Sudipta Saha 2 , Steve Fan 2 , Stephanie Poon 3 , Susanna Mak 4 , Abdul Al-Hesayen 5 , Mustafa Toma 6 , Shelley Zieroth 7 , Kim Anderson 8 , Catherine Demers 9 , Faizan Amin 9 , Liane Porepa 10 , Sharon Chih 11 , Nadia Giannetti 12 , Valeria Rac 13 , Heather J Ross 2 , Gordon H Guyatt 14
JACC: Heart Failure ( IF 10.3 ) Pub Date : 2024-03-27 , DOI: 10.1016/j.jchf.2024.02.009 Ana C Alba 1 , Tayler A Buchan 1 , Sudipta Saha 2 , Steve Fan 2 , Stephanie Poon 3 , Susanna Mak 4 , Abdul Al-Hesayen 5 , Mustafa Toma 6 , Shelley Zieroth 7 , Kim Anderson 8 , Catherine Demers 9 , Faizan Amin 9 , Liane Porepa 10 , Sharon Chih 11 , Nadia Giannetti 12 , Valeria Rac 13 , Heather J Ross 2 , Gordon H Guyatt 14
Affiliation
|
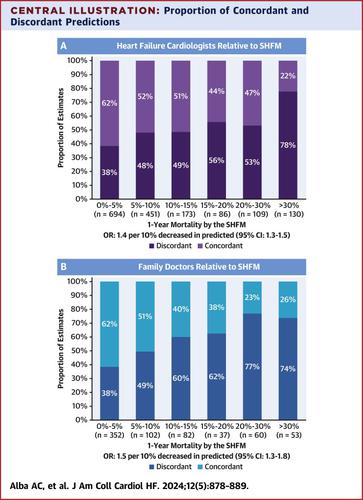
A recent study showed that the accuracy of heart failure (HF) cardiologists and family doctors to predict mortality in outpatients with HF proved suboptimal, performing less well than models. The authors sought to evaluate patient and physician factors associated with physician accuracy. The authors included outpatients with HF from 11 HF clinics. Family doctors and HF cardiologists estimated patient 1-year mortality. They calculated predicted mortality using the Seattle HF Model and followed patients for 1 year to record mortality (or urgent heart transplant or ventricular assist device implant as mortality-equivalent events). Using multivariable logistic regression, the authors evaluated associations among physician experience and confidence in estimates, duration of patient-physician relationship, patient-physician sex concordance, patient race, and predicted risk, with concordant results between physician and model predictions. Among 1,643 patients, 1-year event rate was 10% (95% CI: 8%-12%). One-half of the estimates showed discrepant results between model and physician predictions, mainly owing to physician risk overestimation. Discrepancies were more frequent with increasing patient risk from 38% in low-risk to ∼75% in high-risk patients. When making predictions on male patients, female HF cardiologists were 26% more likely to have discrepant predictions (OR: 0.74; 95% CI: 0.58-0.94). HF cardiologist estimates in Black patients were 33% more likely to be discrepant (OR: 0.67; 95% CI: 0.45-0.99). Low confidence in predictions was associated with discrepancy. Analyses restricted to high-confidence estimates showed inferior calibration to the model, with risk overestimation across risk groups. Discrepant physician and model predictions were more frequent in cases with perceived increased risk. Model predictions outperform physicians even when they are confident in their predictions. (Predicted Prognosis in Heart Failure [INTUITION]; )
中文翻译:

影响医生对左心室射血分数降低的心力衰竭患者预后准确性的因素
最近的一项研究表明,心力衰竭 (HF) 心脏病专家和家庭医生预测心力衰竭门诊患者死亡率的准确性并不理想,表现不如模型。作者试图评估与医生准确性相关的患者和医生因素。作者纳入了来自 11 家心力衰竭诊所的心力衰竭门诊患者。家庭医生和心力衰竭心脏病专家估计了患者的 1 年死亡率。他们使用西雅图 HF 模型计算了预测死亡率,并对患者进行为期 1 年的跟踪记录死亡率(或紧急心脏移植或心室辅助装置植入作为死亡率等效事件)。作者使用多变量逻辑回归,评估了医生经验和估计置信度、医患关系持续时间、医患性别一致性、患者种族和预测风险之间的关联,并且医生和模型预测之间的结果一致。在 1,643 名患者中,1 年事件发生率为 10%(95% CI:8%-12%)。一半的估计显示模型和医生预测之间存在差异,这主要是由于医生风险高估。随着患者风险从低风险患者的 38% 增加到高风险患者的 75%,差异更加频繁。在对男性患者进行预测时,女性心力衰竭心脏病专家做出不一致预测的可能性高出 26%(OR:0.74;95% CI:0.58-0.94)。心脏病专家对黑人患者的心力衰竭估计出现差异的可能性高出 33%(OR:0.67;95% CI:0.45-0.99)。对预测的置信度低与差异相关。仅限于高置信度估计的分析显示模型的校准较差,各个风险组的风险均被高估。 在认为风险增加的病例中,医生和模型的预测不一致的情况更为常见。即使医生对自己的预测充满信心,模型的预测也优于医生。(心力衰竭的预测预后[直觉];)
更新日期:2024-03-27
中文翻译:

影响医生对左心室射血分数降低的心力衰竭患者预后准确性的因素
最近的一项研究表明,心力衰竭 (HF) 心脏病专家和家庭医生预测心力衰竭门诊患者死亡率的准确性并不理想,表现不如模型。作者试图评估与医生准确性相关的患者和医生因素。作者纳入了来自 11 家心力衰竭诊所的心力衰竭门诊患者。家庭医生和心力衰竭心脏病专家估计了患者的 1 年死亡率。他们使用西雅图 HF 模型计算了预测死亡率,并对患者进行为期 1 年的跟踪记录死亡率(或紧急心脏移植或心室辅助装置植入作为死亡率等效事件)。作者使用多变量逻辑回归,评估了医生经验和估计置信度、医患关系持续时间、医患性别一致性、患者种族和预测风险之间的关联,并且医生和模型预测之间的结果一致。在 1,643 名患者中,1 年事件发生率为 10%(95% CI:8%-12%)。一半的估计显示模型和医生预测之间存在差异,这主要是由于医生风险高估。随着患者风险从低风险患者的 38% 增加到高风险患者的 75%,差异更加频繁。在对男性患者进行预测时,女性心力衰竭心脏病专家做出不一致预测的可能性高出 26%(OR:0.74;95% CI:0.58-0.94)。心脏病专家对黑人患者的心力衰竭估计出现差异的可能性高出 33%(OR:0.67;95% CI:0.45-0.99)。对预测的置信度低与差异相关。仅限于高置信度估计的分析显示模型的校准较差,各个风险组的风险均被高估。 在认为风险增加的病例中,医生和模型的预测不一致的情况更为常见。即使医生对自己的预测充满信心,模型的预测也优于医生。(心力衰竭的预测预后[直觉];)











































 京公网安备 11010802027423号
京公网安备 11010802027423号