当前位置:
X-MOL 学术
›
Am. J. Kidney Dis.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
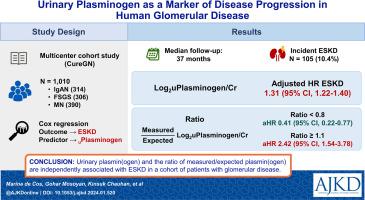
Urinary Plasminogen as a Marker of Disease Progression in Human Glomerular Disease
American Journal of Kidney Diseases ( IF 9.4 ) Pub Date : 2024-03-05 , DOI: 10.1053/j.ajkd.2024.01.520 Marina de Cos 1 , Gohar Mosoyan 1 , Kinsuk Chauhan 1 , Jonathan P Troost 2 , Jenny S Wong 1 , Sean Lefferts 1 , Paul Morgan 1 , Kristin Meliambro 1 , Marc Egerman 1 , Justina Ray 1 , Tom Parker 3 , Daniel Levine 3 , Surya Seshan 4 , Yoni Bardash 5 , Benjamin Horowitz 6 , Candice A Kent 7 , Melissa M Shaw 7 , Alan Perlman 8 , Dennis G Moledina 7 , Steven G Coca 1 , Kirk N Campbell 1
American Journal of Kidney Diseases ( IF 9.4 ) Pub Date : 2024-03-05 , DOI: 10.1053/j.ajkd.2024.01.520 Marina de Cos 1 , Gohar Mosoyan 1 , Kinsuk Chauhan 1 , Jonathan P Troost 2 , Jenny S Wong 1 , Sean Lefferts 1 , Paul Morgan 1 , Kristin Meliambro 1 , Marc Egerman 1 , Justina Ray 1 , Tom Parker 3 , Daniel Levine 3 , Surya Seshan 4 , Yoni Bardash 5 , Benjamin Horowitz 6 , Candice A Kent 7 , Melissa M Shaw 7 , Alan Perlman 8 , Dennis G Moledina 7 , Steven G Coca 1 , Kirk N Campbell 1
Affiliation
|
Glomerular disorders have a highly variable clinical course, and biomarkers that reflect the molecular mechanisms underlying their progression are needed. Based on our previous work identifying plasminogen as a direct cause of podocyte injury, we designed this study to test the association between urine plasmin(ogen) (ie, plasmin and its precursor plasminogen) and end-stage kidney disease (ESKD). Multicenter cohort study. 1,010 patients enrolled in the CureGN Cohort with biopsy-proven glomerular disease (focal segmental glomerulosclerosis, membranous nephropathy, and immunoglobulin A nephropathy). The main predictor was urine plasmin(ogen) at baseline. Levels were measured by an electrochemiluminescent immunoassay developed de novo. Traditional clinical and analytical characteristics were used for adjustment. The ratio of urine plasmin(ogen)/expected plasmin(ogen) was evaluated as a predictor in a separate model. Progression to ESKD. Cox regression was used to examine the association between urinary plasmin(ogen) and time to ESKD. Urinary markers were log transformed to approximate normal distribution and normalized to urinary creatinine (LoguPlasminogen/cr, Log urinary protein/cr [UPCR]). Expected plasmin(ogen) was calculated by multiple linear regression. Adjusted LoguPlasminogen/cr was significantly associated with ESKD (HR per doubling Log uPlasminogen/cr 1.31 [95% CI, 1.22-1.40], <0.001). Comparison of the predictive performance of the models including Log uPlasminogen/cr, Log UPCR, or both markers showed the plasmin(ogen) model superiority. The ratio of measured/expected urine plasmin(ogen) was independently associated with ESKD: HR, 0.41 (95% CI, 0.22-0.77) if ratio<0.8 and HR 2.42 (95% CI, 1.54-3.78) if ratio>1.1 (compared with ratio between 0.8 and 1.1). Single plasmin(ogen) determination does not allow for the study of changes over time. The use of a cohort of mostly white patients and the restriction to patients with 3 glomerular disorders limits the external validity of our analysis. Urinary plasmin(ogen) and the ratio of measured/expected plasmin(ogen) are independently associated with ESKD in a cohort of patients with glomerular disease. Taken together with our previous experimental findings, urinary plasmin(ogen) could be a useful biomarker in prognostic decision making and a target for the development of novel therapies in patients with proteinuria and glomerular disease. Glomerular diseases are an important cause of morbidity and mortality in patients of all ages. Knowing the individual risk of progression to dialysis or transplantation would help to plan the follow-up and treatment of these patients. Our work studies the usefulness of urinary plasminogen as a marker of progression in this context, since previous studies indicate that plasminogen may be involved in the mechanisms responsible for the progression of these disorders. Our work in a sample of 1,010 patients with glomerular disease demonstrates that urinary plasminogen (as well as the ratio of measured to expected plasminogen) is associated with the risk of progression to end-stage kidney disease. Urine plasminogen exhibited good performance and, if further validated, could enable risk stratification for timely interventions in patients with proteinuria and glomerular disease.
中文翻译:

尿纤溶酶原作为人类肾小球疾病进展的标志物
肾小球疾病的临床病程差异很大,需要反映其进展分子机制的生物标志物。基于我们之前确定纤溶酶原是足细胞损伤的直接原因的工作,我们设计了本研究来测试尿纤溶酶(原)(即纤溶酶及其前体纤溶酶原)与终末期肾病(ESKD)之间的关联。多中心队列研究。 CureGN 队列中纳入了 1,010 名经活检证实患有肾小球疾病(局灶节段性肾小球硬化症、膜性肾病和免疫球蛋白 A 肾病)的患者。主要预测因子是基线时的尿纤溶酶(原)。通过从头开发的电化学发光免疫测定法测量水平。使用传统的临床和分析特征进行调整。在单独的模型中评估尿纤溶酶(原)/预期纤溶酶(原)的比率作为预测因子。进展至 ESKD。 Cox 回归用于检查尿纤溶酶(原)与 ESKD 时间之间的关联。将尿液标记物进行对数转换以近似正态分布,并标准化为尿肌酐(Logu纤溶酶原/cr,Log尿蛋白/cr [UPCR])。通过多元线性回归计算预期纤溶酶(原)。调整后的 Logu纤溶酶原/cr 与 ESKD 显着相关(Log u纤溶酶原/cr 每倍增 HR 1.31 [95% CI,1.22-1.40],<0 id=1>1.1(与 0.8 和 1.1 之间的比率相比)。单一纤溶酶(原)测定不允许研究随时间的变化。使用一组主要是白人患者以及对患有 3 种肾小球疾病的患者的限制限制了我们分析的外部有效性。 在一组肾小球疾病患者中,尿纤溶酶(原)和测量/预期纤溶酶(原)的比率与 ESKD 独立相关。结合我们之前的实验结果,尿纤溶酶(原)可能是预后决策中有用的生物标志物,也是开发蛋白尿和肾小球疾病患者新疗法的目标。肾小球疾病是所有年龄段患者发病和死亡的重要原因。了解进展为透析或移植的个体风险将有助于规划这些患者的随访和治疗。我们的工作研究了尿纤溶酶原作为这种情况下进展标志物的有用性,因为之前的研究表明纤溶酶原可能涉及导致这些疾病进展的机制。我们对 1,010 名肾小球疾病患者的样本进行的研究表明,尿纤溶酶原(以及测量的纤溶酶原与预期纤溶酶原的比率)与进展为终末期肾病的风险相关。尿纤溶酶原表现出良好的性能,如果进一步验证,可以对蛋白尿和肾小球疾病患者进行风险分层,以便及时干预。
更新日期:2024-03-05
中文翻译:

尿纤溶酶原作为人类肾小球疾病进展的标志物
肾小球疾病的临床病程差异很大,需要反映其进展分子机制的生物标志物。基于我们之前确定纤溶酶原是足细胞损伤的直接原因的工作,我们设计了本研究来测试尿纤溶酶(原)(即纤溶酶及其前体纤溶酶原)与终末期肾病(ESKD)之间的关联。多中心队列研究。 CureGN 队列中纳入了 1,010 名经活检证实患有肾小球疾病(局灶节段性肾小球硬化症、膜性肾病和免疫球蛋白 A 肾病)的患者。主要预测因子是基线时的尿纤溶酶(原)。通过从头开发的电化学发光免疫测定法测量水平。使用传统的临床和分析特征进行调整。在单独的模型中评估尿纤溶酶(原)/预期纤溶酶(原)的比率作为预测因子。进展至 ESKD。 Cox 回归用于检查尿纤溶酶(原)与 ESKD 时间之间的关联。将尿液标记物进行对数转换以近似正态分布,并标准化为尿肌酐(Logu纤溶酶原/cr,Log尿蛋白/cr [UPCR])。通过多元线性回归计算预期纤溶酶(原)。调整后的 Logu纤溶酶原/cr 与 ESKD 显着相关(Log u纤溶酶原/cr 每倍增 HR 1.31 [95% CI,1.22-1.40],<0 id=1>1.1(与 0.8 和 1.1 之间的比率相比)。单一纤溶酶(原)测定不允许研究随时间的变化。使用一组主要是白人患者以及对患有 3 种肾小球疾病的患者的限制限制了我们分析的外部有效性。 在一组肾小球疾病患者中,尿纤溶酶(原)和测量/预期纤溶酶(原)的比率与 ESKD 独立相关。结合我们之前的实验结果,尿纤溶酶(原)可能是预后决策中有用的生物标志物,也是开发蛋白尿和肾小球疾病患者新疗法的目标。肾小球疾病是所有年龄段患者发病和死亡的重要原因。了解进展为透析或移植的个体风险将有助于规划这些患者的随访和治疗。我们的工作研究了尿纤溶酶原作为这种情况下进展标志物的有用性,因为之前的研究表明纤溶酶原可能涉及导致这些疾病进展的机制。我们对 1,010 名肾小球疾病患者的样本进行的研究表明,尿纤溶酶原(以及测量的纤溶酶原与预期纤溶酶原的比率)与进展为终末期肾病的风险相关。尿纤溶酶原表现出良好的性能,如果进一步验证,可以对蛋白尿和肾小球疾病患者进行风险分层,以便及时干预。
















































 京公网安备 11010802027423号
京公网安备 11010802027423号