JACC: Cardiovascular Interventions ( IF 11.7 ) Pub Date : 2024-01-03 , DOI: 10.1016/j.jcin.2023.10.041 Xavier Armario , Jennifer Carron , Andrew J. Simpkin , Mohamed Elhadi , Ciara Kennedy , Mohamed Abdel-Wahab , Sabine Bleiziffer , Thierry Lefèvre , Alexander Wolf , Thomas Pilgrim , Pedro A. Villablanca , Daniel J. Blackman , Nicolas M. Van Mieghem , Christian Hengstenberg , Martin J. Swaans , Bernard D. Prendergast , Tiffany Patterson , Marco Barbanti , John G. Webb , Miles Behan , Jon Resar , Mao Chen , David Hildick-Smith , Mark S. Spence , David Zweiker , Rodrigo Bagur , Rui Teles , Flavio L. Ribichini , Dariusz Jagielak , Duk-Woo Park , Ran Kornowski , Joanna J. Wykrzykowska , Matjaz Bunc , Rodrigo Estévez-Loureiro , Karl Poon , Matthias Götberg , Raban V. Jeger , Hüseyin Ince , Erik J.S. Packer , Marco Angelillis , Luis Nombela-Franco , Yingqiang Guo , Mikko Savontaus , Abdulrahman M. Al-Moghairi , Catalina Andreea Parasca , Chad Kliger , David Roy , Levente Molnár , Mariana Silva , Jonathon White , Masanori Yamamoto , Pedro Carrilho-Ferreira , Stefan Toggweiler , Vassileios Voudris , Yohei Ohno , Inês Rodrigues , Radosław Parma , Soledad Ojeda , Kostas Toutouzas , Ander Regueiro , Marek Grygier , Khaled AlMerri , Ignacio Cruz-González , Viliam Fridrich , José M. de la Torre Hernández , Stephane Noble , Petr Kala , Lluis Asmarats , Ibrahim Halil Kurt , Johan Bosmans , Martins Erglis , Ivan Casserly , Dounia Iskandarani , Ravinay Bhindi , Joelle Kefer , Wei-Hsian Yin , Liesbeth Rosseel , Hyo-Soo Kim , Stephen O'Connor , Farrel Hellig , Matias Sztejfman , Oscar Mendiz , Andres M. Pineda , Ashok Seth , Elton Pllaha , Fabio S. de Brito , Vilhelmas Bajoras , Mohammed A. Balghith , Michael Lee , Guering Eid-Lidt , Bert Vandeloo , Vinicius Daher Vaz , Mirvat Alasnag , Gian Paolo Ussia , Edgar Tay , Jorge Mayol , Sengottuvelu Gunasekaran , Gennaro Sardella , Wacin Buddhari , Hsien-Li Kao , Antonio Dager , Apostolos Tzikas , Ingibjörg J. Gudmundsdottir , Ahmad Edris , Luis Abel Gutiérrez Jaikel , Eduardo A. Arias , Mohammed Al-Hijji , Mehmet Ertürk , César Conde-Vela , Darko Boljević , Adolfo Ferrero Guadagnoli , Toomas Hermlin , Ahmed M. ElGuindy , Moysés de Oliveira Lima-Filho , Luciano de Moura Santos , Luis Perez , Gabriel Maluenda , Ali Rıza Akyüz , Imad A. Alhaddad , Haitham Amin , Chak-Yu So , Arif A. Al Nooryani , Carlos Vaca , Juan Albistur , Quang Ngoc Nguyen , Dabit Arzamendi , Eberhard Grube , Thomas Modine , Didier Tchétché , Kentaro Hayashida , Azeem Latib , Raj R. Makkar , Nicolo Piazza , Lars Søndergaard , John William McEvoy , Darren Mylotte
|
Background
The COVID-19 pandemic adversely affected health care systems. Patients in need of transcatheter aortic valve replacement (TAVR) are especially susceptible to treatment delays.
Objectives
The study sought to evaluate the impact of the COVID-19 pandemic on global TAVR activity.
Methods
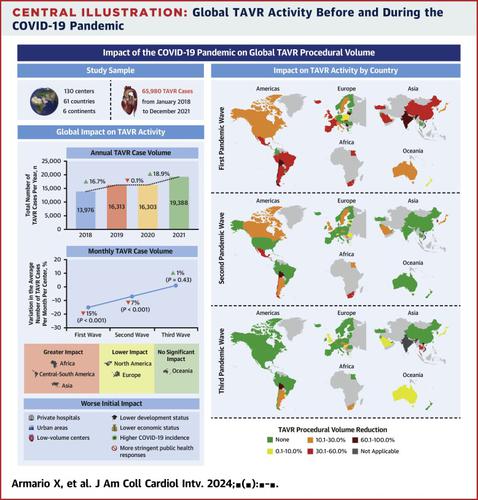
This international registry reported monthly TAVR case volume in participating institutions prior to and during the COVID-19 pandemic (January 2018 to December 2021). Hospital-level information on public vs private, urban vs rural, and TAVR volume was collected, as was country-level information on socioeconomic status, COVID-19 incidence, and governmental public health responses.
Results
We included 130 centers from 61 countries, including 65,980 TAVR procedures. The first and second pandemic waves were associated with a significant reduction of 15% (P < 0.001) and 7% (P < 0.001) in monthly TAVR case volume, respectively, compared with the prepandemic period. The third pandemic wave was not associated with reduced TAVR activity. A greater reduction in TAVR activity was observed in Africa (−52%; P = 0.001), Central-South America (−33%; P < 0.001), and Asia (−29%; P < 0.001). Private hospitals (P = 0.005), urban areas (P = 0.011), low-volume centers (P = 0.002), countries with lower development (P < 0.001) and economic status (P < 0.001), higher COVID-19 incidence (P < 0.001), and more stringent public health restrictions (P < 0.001) experienced a greater reduction in TAVR activity.
Conclusions
TAVR procedural volume declined substantially during the first and second waves of the COVID-19 pandemic, especially in Africa, Central-South America, and Asia. National socioeconomic status, COVID-19 incidence, and public health responses were associated with treatment delays. This information should inform public health policy in case of future global health crises.
中文翻译:

COVID-19 大流行对全球 TAVR 活动的影响:COVID-TAVI 研究
背景
COVID-19 大流行对医疗保健系统产生了不利影响。需要经导管主动脉瓣置换术(TAVR)的患者特别容易受到治疗延误的影响。
目标
该研究旨在评估 COVID-19 大流行对全球 TAVR 活动的影响。
方法
该国际登记处报告了参与机构在 COVID-19 大流行之前和期间(2018 年 1 月至 2021 年 12 月)的每月 TAVR 病例数。收集了有关公立与私立、城市与农村以及 TAVR 数量的医院层面信息,以及有关社会经济状况、COVID-19 发病率和政府公共卫生应对措施的国家层面信息。
结果
我们纳入了来自 61 个国家的 130 个中心,包括 65,980 例 TAVR 手术。与大流行前相比,第一波和第二波大流行导致每月 TAVR 病例数分别显着减少 15% ( P < 0.001) 和 7% ( P < 0.001)。第三波大流行与 TAVR 活动减少无关。非洲(−52%; P = 0.001)、中南美洲(−33%; P < 0.001)和亚洲(−29%; P < 0.001)的 TAVR 活动下降幅度更大。私立医院 ( P = 0.005)、城市地区 ( P = 0.011)、低流量中心 ( P = 0.002)、发展水平较低 ( P < 0.001) 和经济状况较低的国家 ( P < 0.001)、COVID-19 较高的国家发生率 ( P < 0.001) 和更严格的公共卫生限制 ( P < 0.001) 经历了 TAVR 活动的更大减少。
结论
在 COVID-19 大流行的第一波和第二波期间,TAVR 手术量大幅下降,特别是在非洲、中南美洲和亚洲。国家社会经济状况、COVID-19 发病率和公共卫生反应与治疗延误有关。这些信息应为公共卫生政策提供信息,以防未来发生全球健康危机。






























 京公网安备 11010802027423号
京公网安备 11010802027423号