Clinical Lung Cancer ( IF 3.3 ) Pub Date : 2023-12-28 , DOI: 10.1016/j.cllc.2023.12.007 Frank Detterbeck 1 , Sora Ely 2 , Brooks Udelsman 3 , Justin Blasberg 1 , Daniel Boffa 1 , Andrew Dhanasopon 1 , Vincnet Mase 1 , Gavitt Woodard 1
|
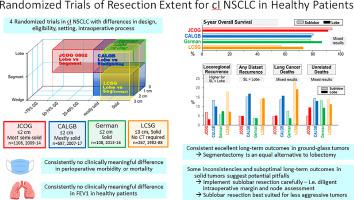
Lobectomy has been the standard treatment for stage I lung cancer in healthy patients, largely based on a randomized trial published in 1995. Nevertheless, research has continued regarding the role of sublobar resection. Three additional randomized trials addressing resection extent in healthy patients have recently been published. These 4 trials involve differences in design, eligibility, interventions, and intraoperative processes. Patients were ineligible if intraoperative assessment demonstrated stage >IA or inadequate resection margins. All trials consistently show no differences in perioperative morbidity, mortality, and postoperative changes in lung function between sublobar resection and lobectomy - consistent with other non-randomized evidence. Long-term outcomes are generally encouraging of lesser resection, but some inconsistencies are apparent. The 2 larger recent trials demonstrated no overall survival difference while the others suggested better survival after lobectomy vs sublobar resection. Recurrence-free survival was found to be the same after lobectomy vs sublobar resection in 3 trials, despite higher locoregional recurrences after sublobar resection. The low 5-year recurrence-free survival (64%, regardless of resection extent) in one recent trial highlights the need for further optimization.
Thus, there is high-level evidence that sublobar resection is a reasonable alternative to lobectomy in healthy patients. However, variability in long-term results suggests that aspects of patients, tumors and interventions need to be better understood. Therefore, we propose to apply sublobar resection cautiously; especially because there are no short-term benefits. Sublobar resection requires careful attention to intraoperative details (nodes, margins), and may be best suited for less aggressive (e.g., ground glass, slow growing) tumors.
中文翻译:

现在我们知道了——对 I 期肺癌切除范围的思考
肺叶切除术一直是健康患者 I 期肺癌的标准治疗方法,主要基于 1995 年发表的一项随机试验。尽管如此,关于亚肺叶切除术的作用的研究仍在继续。最近还发表了另外三项针对健康患者切除范围的随机试验。这 4 项试验涉及设计、资格、干预措施和术中过程方面的差异。如果术中评估显示分期 >IA 或切除边缘不足,则患者不符合资格。所有试验一致显示,亚肺叶切除术和肺叶切除术在围手术期发病率、死亡率和术后肺功能变化方面没有差异,这与其他非随机证据一致。较小切除的长期结果通常令人鼓舞,但也存在一些明显的不一致之处。最近两项较大的试验表明总体生存率没有差异,而其他试验则表明肺叶切除术后的生存率优于亚肺叶切除术后的生存率。 3 项试验发现,肺叶切除术与亚肺叶切除术后的无复发生存率相同,尽管亚肺叶切除术后的局部区域复发率较高。最近的一项试验显示,5 年无复发生存率较低(64%,无论切除范围如何),凸显了进一步优化的必要性。
因此,有大量证据表明,对于健康患者来说,亚肺叶切除术是肺叶切除术的合理替代方案。然而,长期结果的可变性表明,需要更好地了解患者、肿瘤和干预措施的各个方面。因此,我们建议谨慎应用亚肺叶切除术;尤其是因为没有短期利益。亚肺叶切除术需要仔细注意术中细节(淋巴结、切缘),并且可能最适合侵袭性较小的肿瘤(例如毛玻璃状肿瘤、生长缓慢的肿瘤)。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号