JACC: Heart Failure ( IF 10.3 ) Pub Date : 2023-10-18 , DOI: 10.1016/j.jchf.2023.07.030
Andrew Wang 1 , John A Spertus 2 , Daniel M Wojdyla 3 , Theodore P Abraham 4 , Ester Kim Nilles 3 , Anjali Tiku Owens 5 , Sara Saberi 6 , Sharon Cresci 7 , Amy Sehnert 8 , Neal K Lakdawala 9
|
Background
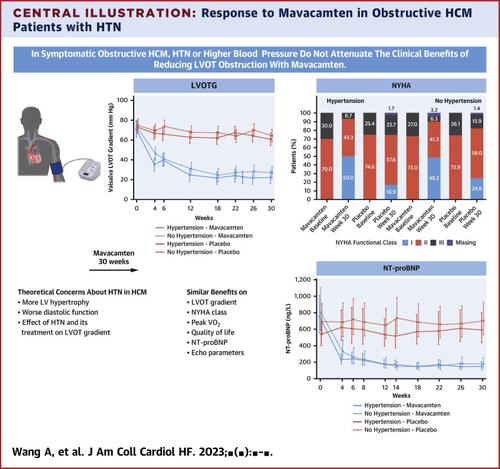
Hypertension (HTN) is common in patients with hypertrophic cardiomyopathy (HCM), but its effect on the treatment of left ventricular outflow tract (LVOT) obstruction is undefined. Although elevated systolic blood pressure (SBP) may impact dynamic LVOT gradients, its response to cardiac myosin inhibition is unknown.
Objectives
In a post hoc exploratory analysis of the EXPLORER-HCM trial (Clinical Study to Evaluate Mavacamten [MYK-461] in Adults With Symptomatic Obstructive Hypertrophic Cardiomyopathy), the authors examined the characteristics of patients with obstructive HCM and HTN and the associations between HTN, SBP, and the response to mavacamten treatment of LVOT obstruction.
Methods
Patients were stratified by baseline history of HTN and mean SBP during 30-week treatment with mavacamten or placebo. The study estimated treatment differences and evaluated HTN and SBP groups by treatment interaction. Analysis of covariance was used to model changes in continuous endpoints, and a generalized linear model was used for binary endpoints.
Results
HTN was present in 119 of 251 patients (47.4%), including 60 receiving mavacamten and 59 receiving placebo. Patients with HTN vs no HTN were older (63.4 vs 54.0 years; P < 0.001), had higher SBP (134 ± 15.1 mm Hg vs 123 ± 13.8 mm Hg; P < 0.001), more comorbidities, and lower peak oxygen consumption (19 ± 3 vs 20 ± 4 mL/kg/min; P = 0.021). Patients with HTN had similar NYHA functional class (NYHA functional class II, 72% vs 73%), Valsalva LVOT gradients (72 ± 34 mm Hg vs 74 ± 30 mm Hg), Kansas City Cardiomyopathy Questionnaire–Clinical Summary Scores (70.6 ± 18.8 vs 68.9 ± 23.1), and NT pro–B-type natriuretic peptide levels (geometric mean 632 ± 129 pg/mL vs 745 ± 130 pg/mL). Mavacamten-treated patients had improvement in all primary, secondary, and exploratory endpoints regardless of HTN status or mean SBP.
Conclusions
The clinical benefits of mavacamten in symptomatic, obstructive HCM were similar in patients with and without HTN, despite differences in baseline characteristics. (Clinical Study to Evaluate Mavacamten [MYK-461] in Adults With Symptomatic Obstructive Hypertrophic Cardiomyopathy [EXPLORER-HCM]; NCT03470545)
中文翻译:

Mavacamten 治疗伴有或不伴有高血压的梗阻性肥厚性心肌病:EXPLORER-HCM 试验的事后分析
背景
高血压(HTN)在肥厚型心肌病(HCM)患者中很常见,但其对左心室流出道(LVOT)梗阻治疗的影响尚不清楚。尽管收缩压(SBP) 升高可能会影响动态 LVOT 梯度,但其对心肌肌球蛋白抑制的反应尚不清楚。
目标
在 EXPLORER-HCM 试验(评估 Mavacamten [MYK-461] 在成人症状性梗阻性肥厚性心肌病患者中的临床研究)的事后探索性分析中,作者检查了梗阻性 HCM 和 HTN 患者的特征以及 HTN、 SBP 以及 mavacamten 治疗 LVOT 梗阻的反应。
方法
根据 mavacamten 或安慰剂治疗 30 周期间的基线 HTN 病史和平均 SBP 对患者进行分层。该研究估计了治疗差异,并通过治疗相互作用评估了 HTN 和 SBP 组。协方差分析用于模拟连续端点的变化,广义线性模型用于二元端点。
结果
251 名患者中有 119 名(47.4%)存在高血压,其中 60 名接受 mavacamten 治疗的患者和 59 名接受安慰剂的患者。患有 HTN 的患者与无 HTN 的患者相比,年龄较大(63.4 岁 vs 54.0 岁; P < 0.001),SBP 较高(134 ± 15.1 mm Hg vs 123 ± 13.8 mm Hg; P < 0.001),合并症较多,峰值耗氧量较低(19 ± 3 与 20 ± 4 毫升/公斤/分钟; P = 0.021)。 HTN 患者具有相似的 NYHA 功能分级(NYHA 功能分级 II,72% vs 73%)、Valsalva LVOT 梯度(72 ± 34 mm Hg vs 74 ± 30 mm Hg)、堪萨斯城心肌病问卷临床总结评分(70.6 ± 18.8) vs 68.9 ± 23.1)和 NT pro-B 型利钠肽水平(几何平均值 632 ± 129 pg/mL vs 745 ± 130 pg/mL)。无论 HTN 状态或平均收缩压如何,接受 Mavacamten 治疗的患者在所有主要、次要和探索性终点方面都有改善。
结论
尽管基线特征存在差异,但患有和不患有 HTN 的患者中,mavacamten 对有症状、梗阻性 HCM 的临床益处相似。 (评估 Mavacamten [MYK-461] 在成人症状性梗阻性肥厚性心肌病 [EXPLORER-HCM] 中的临床研究; NCT03470545 )

































 京公网安备 11010802027423号
京公网安备 11010802027423号