Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2023-10-02 , DOI: 10.1016/j.jacc.2023.08.006 Hasan K Siddiqi 1 , John Trahanas 2 , Meng Xu 3 , Quinn Wells 1 , Eric Farber-Eger 1 , Chetan Pasrija 2 , Kaushik Amancherla 1 , Alexandra Debose-Scarlett 2 , D Marshall Brinkley 1 , JoAnn Lindenfeld 1 , Jonathan N Menachem 1 , Henry Ooi 4 , Dawn Pedrotty 4 , Lynn Punnoose 1 , Aniket S Rali 1 , Suzanne Sacks 1 , Mark Wigger 4 , Sandip Zalawadiya 1 , William McMaster 2 , Steven Devries 2 , Ashish Shah 2 , Kelly Schlendorf 1
|
Background
Heart transplantation using donation after circulatory death (DCD) allografts is increasingly common, expanding the donor pool and reducing transplant wait times. However, data remain limited on clinical outcomes.
Objectives
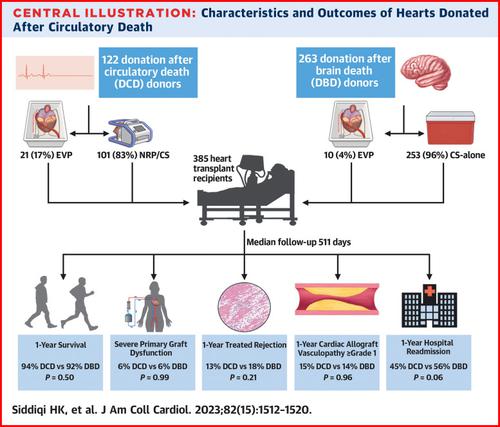
We sought to compare 6-month and 1-year clinical outcomes between recipients of DCD hearts, most of them recovered with the use of normothermic regional perfusion (NRP), and recipients of donation after brain death (DBD) hearts.
Methods
We conducted a single-center retrospective observational study of all adult heart-only transplants from January 2020 to January 2023. Recipient and donor data were abstracted from medical records and the United Network for Organ Sharing registry, respectively. Survival analysis and Cox regression were used to compare the groups.
Results
During the study period, 385 adults (median age 57.4 years [IQR: 48.0-63.7 years]) underwent heart-only transplantation, including 122 (32%) from DCD donors, 83% of which were recovered with the use of NRP. DCD donors were younger and had fewer comorbidities than DBD donors. DCD recipients were less often hospitalized before transplantation and less likely to require pretransplantation temporary mechanical circulatory support compared with DBD recipients. There were no significant differences between groups in 1-year survival, incidence of severe primary graft dysfunction, treated rejection during the first year, or likelihood of cardiac allograft vasculopathy at 1 year after transplantation.
Conclusions
In the largest single-center comparison of DCD and DBD heart transplantations to date, outcomes among DCD recipients are noninferior to those of DBD recipients. This study adds to the published data supporting DCD donors as a safe means to expand the heart donor pool.
中文翻译:

循环死亡后心脏移植捐赠的结果
背景
使用循环死亡后捐献(DCD)同种异体移植的心脏移植越来越普遍,扩大了捐献者库并减少了移植等待时间。然而,关于临床结果的数据仍然有限。
目标
我们试图比较 DCD 心脏接受者和脑死亡捐赠 (DBD) 心脏接受者之间 6 个月和 1 年的临床结果,其中大多数通过常温局部灌注 (NRP) 恢复。
方法
我们对 2020 年 1 月至 2023 年 1 月期间所有成人仅心脏移植进行了单中心回顾性观察研究。受者和供者数据分别从医疗记录和器官共享联合网络登记处提取。使用生存分析和Cox回归来比较各组。
结果
研究期间,385 名成年人(中位年龄 57.4 岁 [IQR:48.0-63.7 岁])接受了纯心脏移植,其中 122 名(32%)来自 DCD 捐赠者,其中 83% 通过使用 NRP 得以康复。DCD 捐献者比 DBD 捐献者更年轻,合并症也更少。与 DBD 受者相比,DCD 受者在移植前住院的频率较低,并且不太可能需要移植前临时机械循环支持。各组之间的 1 年生存率、严重原发性移植物功能障碍的发生率、第一年的排斥反应或移植后 1 年出现心脏同种异体移植血管病变的可能性没有显着差异。
结论
在迄今为止 DCD 和 DBD 心脏移植的最大单中心比较中,DCD 接受者的结果并不劣于 DBD 接受者。这项研究增加了已发表的数据,支持 DCD 捐献者作为扩大心脏捐献者库的安全手段。

































 京公网安备 11010802027423号
京公网安备 11010802027423号