Environment International ( IF 10.3 ) Pub Date : 2022-10-19 , DOI: 10.1016/j.envint.2022.107594 Tingfan Jin 1 , Qian Di 2 , Weeberb J Réquia 3 , Mahdieh Danesh Yazdi 4 , Edgar Castro 1 , Tszshan Ma 5 , Yifan Wang 5 , Haisu Zhang 5 , Liuhua Shi 5 , Joel Schwartz 1
|
Background & aim
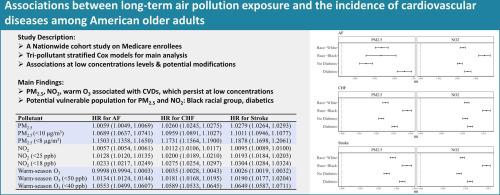
Numerous studies have linked air pollution with cardiovascular diseases. Fewer studies examined the associations at low concentration levels or assessed potential modifiers. Some investigations only examined hospitalizations, which can miss incident cases. This study aims to address these gaps through a nationwide cohort study of Medicare enrollees.
Methods
Our study cohort comprise all Medicare enrollees (≥65 years old) continuously enrolled in the fee-for-service program and both Medicare part A and B across the contiguous U.S. from 2000 to 2016. We examined the associations of population-weighted ZIP code-level annual average PM2.5, NO2, and warm-season O3 (May-October), with the first diagnoses of atrial fibrillation (AF), congestive heart failure (CHF), and stroke. We fit multi-pollutant Cox proportional hazards models adjusted for individual demographic characteristics and area-level covariates. We further examined these associations at low pollutant concentration levels and the potential effect modifications by race/ethnicity and comorbidities (diabetes, hypertension, hyperlipidemia).
Results
Elevated PM2.5 and NO2 levels were associated with increased incidence of AF, CHF, and stroke. For each 1 μg/m3 increase in annual PM2.5, hazard ratios (HRs) were 1.0059 (95%CI: 1.0054-1.0064), 1.0260 (95%CI: 1.0256-1.0264), and 1.0279 (95%CI: 1.0274-1.0284), respectively. For each1 ppb increase in annual NO2, HRs are 1.0057 (95%CI: 1.0056-1.0059), 1.0112 (95%CI: 1.0110-1.0113), and 1.0095 (95%CI: 1.0093-1.0096), respectively. For warm-season O3, each 1 ppb increase was associated with increased incidence of CHF (HR=1.0035, 95%CI: 1.0033–1.0037) and stroke (HR=1.0026, 95%CI: 1.0023–1.0028). Larger magnitudes of HRs were observed when restricted to pollutants levels lower than NAAQS standards. Generally higher risks were observed for Black people and diabetics.
Conclusions
Long-term exposure to PM2.5, NO2, and warm-season O3 were associated with increased incidence of cardiovascular diseases, even at low pollutant concentration levels. Black people and people with diabetes were found to be vulnerable populations.
中文翻译:

美国老年人长期接触空气污染与心血管疾病发病率的关系
背景与目标
许多研究已将空气污染与心血管疾病联系起来。很少有研究检查低浓度水平下的关联或评估潜在的修饰因素。一些调查只检查住院情况,这可能会遗漏事故病例。本研究旨在通过针对医疗保险参保者的全国性队列研究来解决这些差距。
方法
我们的研究队列包括 2000 年至 2016 年间美国本土连续参加按服务付费计划以及 Medicare A 部分和 B 部分的所有 Medicare 参保者(≥65 岁)。我们研究了人口加权邮政编码之间的关联:年平均 PM 2.5 、NO 2和暖季 O 3 (5 月至 10 月)水平,首次诊断为心房颤动 (AF)、充血性心力衰竭 (CHF) 和中风。我们拟合了根据个人人口特征和区域级协变量进行调整的多污染物 Cox 比例风险模型。我们进一步研究了低污染物浓度水平下的这些关联以及种族/民族和合并症(糖尿病、高血压、高脂血症)的潜在影响。
结果
PM 2.5和 NO 2水平升高与 AF、CHF 和中风的发病率增加相关。年 PM 2.5每增加 1 μg/m 3 ,风险比 (HR) 分别为 1.0059 (95%CI: 1.0054-1.0064)、1.0260 (95%CI: 1.0256-1.0264) 和 1.0279 (95%CI: 1.0274-1.0274)。 1.0284),分别。每年 NO 2每增加 1 ppb,HR 分别为 1.0057 (95% CI: 1.0056-1.0059)、1.0112 (95% CI: 1.0110-1.0113) 和 1.0095 (95% CI: 1.0093-1.0096)。对于暖季O 3 ,每增加1 ppb,CHF(HR=1.0035,95%CI:1.0033–1.0037)和中风(HR=1.0026,95%CI:1.0023–1.0028)发病率增加相关。当污染物水平低于 NAAQS 标准时,会观察到更大幅度的 HR。一般来说,黑人和糖尿病患者的风险较高。
结论
长期接触PM 2.5 、NO 2和暖季O 3与心血管疾病发病率增加有关,即使在污染物浓度水平较低的情况下也是如此。黑人和糖尿病患者被发现是弱势群体。

































 京公网安备 11010802027423号
京公网安备 11010802027423号