CardioVascular and Interventional Radiology ( IF 2.8 ) Pub Date : 2022-08-24 , DOI: 10.1007/s00270-022-03222-y Malte Maria Sieren 1, 2 , Julian Pfarr 1 , Schekeb Aludin 3 , Karim Mostafa 3 , Erik Stahlberg 1, 2 , Franz Wegner 1, 2 , Sam Mogadas 1, 2 , Rene Rusch 4 , Marco Horn 5 , Philipp Schäfer 1
|
Objective
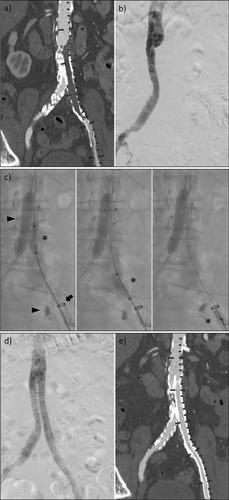
Thrombectomy of the aortoiliac segment remains a challenge for surgical and endovascular revision. This study aimed to evaluate the concept of percutaneous thrombectomy in patients with aortoiliac segment occlusions.
Materials & Methods
Eighteen patients with aortoiliac occlusion who underwent percutaneous thrombectomy were retrospectively identified using the local picture archive and divided into the stent-graft (N = 10) and native vessels (N = 8) groups. The procedure was performed by placing a 12–24 French sheath adjacent to the distal end of the occluded vessel segment. The occlusion was passed with a balloon catheter which was retracted after inflation, to deliver the thrombus into the sheath. Technical success (reperfusion of the vessel and no residual thrombus/stenosis < 30%), complications and primary arterial patency were assessed. Follow-up included computed tomography angiography and evaluation of the clinical situation via telephone.
Results
Technical success was achieved in 38% (7/18) of patients after percutaneous thrombectomy alone and in 100% after additional procedures. The most common complication was peripheral embolism (44%, 8/18), which was treated successfully in all cases and was linked to a mismatch between the sheath and target vessel of ≥ 1 mm (P < .01). There were no significant differences in the incidence of complications between the two groups. Primary patency was 72% (13/18) with no significant difference between groups (P = .94). Follow-up CT scans were available for 13/18 patients (72%), with a mean follow-up time of 270 ± 146 days. All patients were contacted via phone (follow-up time, 653 ± 264 days).
Conclusion
Percutaneous thrombectomy appears to be effective for revascularization of the aortoiliac segment, both in stent-grafts and in native vessels. The most common complication is peripheral embolism; however, the risk may be reduced by choosing an adequate sheath size.
中文翻译:

主动脉髂段闭塞患者的经皮血栓切除术:病例系列
客观的
主动脉髂段的血栓切除术仍然是手术和血管内修复的挑战。本研究旨在评估主动脉髂段闭塞患者经皮血栓切除术的概念。
材料与方法
18 例接受经皮取栓术的主髂动脉闭塞患者使用当地图片档案进行回顾性识别,并分为支架移植组(N = 10)和自体血管组(N = 8)。通过在闭塞血管段的远端附近放置一个 12-24 French 护套来执行该程序。用膨胀后缩回的球囊导管通过闭塞,以将血栓输送到护套中。评估了技术成功(血管再灌注和无残留血栓/狭窄 < 30%)、并发症和原发动脉通畅情况。随访包括计算机断层扫描血管造影和通过电话评估临床情况。
结果
38% (7/18) 的患者在单独进行经皮血栓切除术后取得了技术成功,在额外的手术后取得了 100% 的技术成功。最常见的并发症是外周栓塞 (44%, 8/18),所有病例均成功治疗,并且与鞘管和靶血管之间的不匹配≥ 1 mm ( P < .01)。两组并发症发生率无显着差异。主要通畅率为 72% (13/18),组间无显着差异 ( P = .94)。13/18 名患者 (72%) 可获得随访 CT 扫描,平均随访时间为 270 ± 146 天。所有患者均通过电话联系(随访时间为 653 ± 264 天)。
结论
经皮血栓切除术似乎对主动脉瓣段的血运重建有效,无论是在支架移植物中还是在天然血管中。最常见的并发症是外周栓塞;但是,通过选择合适的护套尺寸可以降低风险。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号