Surgical Endoscopy ( IF 2.4 ) Pub Date : 2022-08-03 , DOI: 10.1007/s00464-022-09493-3 Davit L Aghayan 1, 2 , Gabriella d'Albenzio 1, 3 , Åsmund A Fretland 1, 4, 5 , Egidijus Pelanis 1, 4 , Bård I Røsok 5 , Sheraz Yaqub 4, 5 , Rafael Palomar 1, 6 , Bjørn Edwin 1, 4, 5
|
Background
Traditionally, patients with large liver tumors (≥ 50 mm) have been considered for anatomic major hepatectomy. Laparoscopic resection of large liver lesions is technically challenging and often performed by surgeons with extensive experience. The current study aimed to evaluate the surgical and oncologic safety of laparoscopic parenchyma-sparing liver resection in patients with large colorectal metastases.
Methods
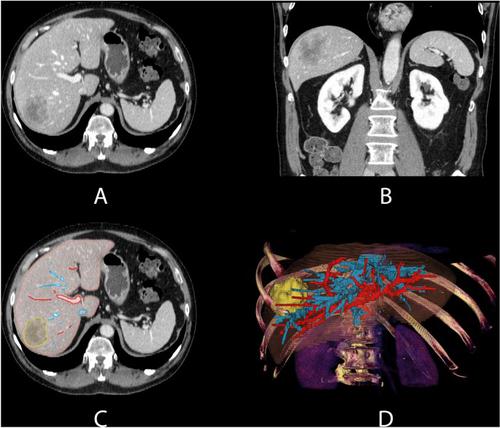
Patients who primarily underwent laparoscopic parenchyma-sparing liver resection (less than 3 consecutive liver segments) for colorectal liver metastases between 1999 and 2019 at Oslo University Hospital were analyzed. In some recent cases, a computer-assisted surgical planning system was used to better visualize and understand the patients’ liver anatomy, as well as a tool to further improve the resection strategy. The surgical and oncologic outcomes of patients with large (≥ 50 mm) and small (< 50 mm) tumors were compared. Multivariable Cox-regression analysis was performed to identify risk factors for survival.
Results
In total 587 patients met the inclusion criteria (large tumor group, n = 59; and small tumor group, n = 528). Median tumor size was 60 mm (range, 50–110) in the large tumor group and 21 mm (3–48) in the small tumor group (p < 0.001). Patient age and CEA level were higher in the large tumor group (8.4 μg/L vs. 4.6 μg/L, p < 0.001). Operation time and conversion rate were similar, while median blood loss was higher in the large tumor group (500 ml vs. 200 ml, p < 0.001). Patients in the large tumor group had shorter 5 year overall survival (34% vs 49%, p = 0.027). However, in the multivariable Cox-regression analysis tumor size did not impact survival, unlike parameters such as age, ASA score, CEA level, extrahepatic disease at liver surgery, and positive lymph nodes in the primary tumor.
Conclusion
Laparoscopic parenchyma-sparing resections for large colorectal liver metastases provide satisfactory short and long-term outcomes.
Graphical abstract
中文翻译:

大(≥ 50 mm)结直肠转移瘤的腹腔镜保肝实质肝切除术
背景
传统上,大型肝脏肿瘤(≥ 50 mm)的患者被考虑进行解剖性大肝切除术。大型肝脏病灶的腹腔镜切除术在技术上具有挑战性,通常由经验丰富的外科医生执行。目前的研究旨在评估大结直肠转移患者腹腔镜保留实质肝切除术的手术和肿瘤学安全性。
方法
分析了 1999 年至 2019 年间在奥斯陆大学医院接受腹腔镜保留实质肝切除术(少于 3 个连续肝段)以治疗结直肠癌肝转移的患者。在最近的一些案例中,计算机辅助手术计划系统被用于更好地可视化和理解患者的肝脏解剖结构,以及进一步改进切除策略的工具。比较了大肿瘤(≥ 50 毫米)和小肿瘤(< 50 毫米)患者的手术和肿瘤学结果。进行多变量 Cox 回归分析以确定生存的危险因素。
结果
共有 587 名患者符合纳入标准(大肿瘤组,n = 59;小肿瘤组,n = 528)。大肿瘤组的中位肿瘤大小为 60 毫米(范围 50-110),小肿瘤组为 21 毫米(3-48)(p < 0.001)。大肿瘤组的患者年龄和 CEA 水平更高(8.4 μg/L 对比 4.6 μg/L,p < 0.001)。手术时间和转化率相似,而大肿瘤组的中位失血量更高(500 毫升对 200 毫升,p < 0.001)。大肿瘤组患者的 5 年总生存期较短(34% 对 49%,p = 0.027)。然而,在多变量 Cox 回归分析中,肿瘤大小不影响生存,这与年龄、ASA 评分、CEA 水平、肝脏手术时的肝外疾病和原发肿瘤淋巴结阳性等参数不同。
结论
大结直肠肝转移的腹腔镜保留实质切除术可提供令人满意的短期和长期结果。






























 京公网安备 11010802027423号
京公网安备 11010802027423号