当前位置:
X-MOL 学术
›
Cancer Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Spirometry at diagnosis and overall survival in non-small cell lung cancer patients
Cancer Medicine ( IF 2.9 ) Pub Date : 2022-05-12 , DOI: 10.1002/cam4.4808 Ting Zhai 1 , Yi Li 2 , Robert Brown 3 , Michael Lanuti 4 , Justin F Gainor 5 , David C Christiani 1, 3
Cancer Medicine ( IF 2.9 ) Pub Date : 2022-05-12 , DOI: 10.1002/cam4.4808 Ting Zhai 1 , Yi Li 2 , Robert Brown 3 , Michael Lanuti 4 , Justin F Gainor 5 , David C Christiani 1, 3
Affiliation
|
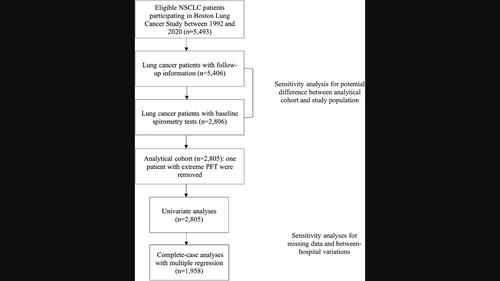
Pulmonary function can predict all-cause mortality, and chronic obstructive pulmonary disease (COPD) is associated with worse overall survival (OS) in non-small cell lung cancer (NSCLC) patients. Though pre-operative lung function is predictive of in-hospital mortality following lung cancer surgery, its predictive utility for long-term survival is unclear. The prognostic role of commonly used spirometry tests in survival of lung cancer also remains uncertain. This study evaluates the role of spirometry at lung cancer diagnosis in predicting OS of NSCLC patients. This was a retrospective study using data from the Boston Lung Cancer Study on newly diagnosed NSCLC patients with spirometry tests performed before cancer therapy (n = 2805). Spirometric test values, after being categorized using quartiles, were analyzed for association with OS using univariate and risk-adjusted multiple regression models. Further, we analyzed OS by the status of COPD determined by spirometry, and, among those with COPD, by its stage defined by the Global Initiative for Chronic Obstructive Lung Disease criteria. Both univariate and multiple regression models demonstrated that lower quartiles of actual and percent predicted forced expiratory volume in 1 second and forced vital capacity at lung cancer diagnosis were significantly associated with worse OS. Spirometry-determined COPD, and more advanced stage of COPD at lung cancer diagnosis were associated with worse lung cancer OS. The findings provide evidence that a good pulmonary function at diagnosis may help improve OS in NSCLC patients.
中文翻译:

非小细胞肺癌患者诊断时的肺活量测定和总生存期
肺功能可以预测全因死亡率,慢性阻塞性肺病 (COPD) 与非小细胞肺癌 (NSCLC) 患者较差的总生存期 (OS) 相关。尽管术前肺功能可预测肺癌手术后的院内死亡率,但其对长期生存的预测效用尚不清楚。常用的肺活量测定法在肺癌生存中的预后作用也仍不确定。本研究评估了肺活量测定法在肺癌诊断中预测 NSCLC 患者 OS 的作用。这是一项回顾性研究,使用波士顿肺癌研究的数据对新诊断的 NSCLC 患者进行癌症治疗前进行的肺活量测定(n = 2805)。在使用四分位数分类后,使用单变量和风险调整的多元回归模型分析肺活量测试值与 OS 的关联。此外,我们通过肺活量测定法确定的 COPD 状态分析 OS,并且在 COPD 患者中,根据慢性阻塞性肺病全球倡议标准定义的阶段分析 OS。单变量和多元回归模型均表明,肺癌诊断时 1 秒用力呼气量和用力肺活量的实际和预测百分比的较低四分位数与较差的 OS 显着相关。肺活量测定法确定的 COPD 和肺癌诊断时更晚期的 COPD 与较差的肺癌 OS 相关。这些发现提供的证据表明,诊断时良好的肺功能可能有助于改善 NSCLC 患者的 OS。
更新日期:2022-05-12
中文翻译:

非小细胞肺癌患者诊断时的肺活量测定和总生存期
肺功能可以预测全因死亡率,慢性阻塞性肺病 (COPD) 与非小细胞肺癌 (NSCLC) 患者较差的总生存期 (OS) 相关。尽管术前肺功能可预测肺癌手术后的院内死亡率,但其对长期生存的预测效用尚不清楚。常用的肺活量测定法在肺癌生存中的预后作用也仍不确定。本研究评估了肺活量测定法在肺癌诊断中预测 NSCLC 患者 OS 的作用。这是一项回顾性研究,使用波士顿肺癌研究的数据对新诊断的 NSCLC 患者进行癌症治疗前进行的肺活量测定(n = 2805)。在使用四分位数分类后,使用单变量和风险调整的多元回归模型分析肺活量测试值与 OS 的关联。此外,我们通过肺活量测定法确定的 COPD 状态分析 OS,并且在 COPD 患者中,根据慢性阻塞性肺病全球倡议标准定义的阶段分析 OS。单变量和多元回归模型均表明,肺癌诊断时 1 秒用力呼气量和用力肺活量的实际和预测百分比的较低四分位数与较差的 OS 显着相关。肺活量测定法确定的 COPD 和肺癌诊断时更晚期的 COPD 与较差的肺癌 OS 相关。这些发现提供的证据表明,诊断时良好的肺功能可能有助于改善 NSCLC 患者的 OS。

































 京公网安备 11010802027423号
京公网安备 11010802027423号