当前位置:
X-MOL 学术
›
J. Leukoc. Biol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
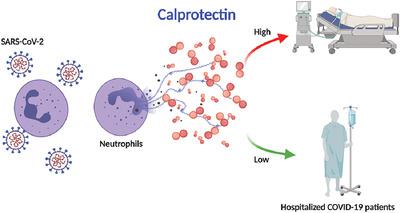
Neutrophil calprotectin identifies severe pulmonary disease in COVID-19.
Journal of Leukocyte Biology ( IF 3.6 ) Pub Date : 2020-09-01 , DOI: 10.1002/jlb.3covcra0720-359r Hui Shi 1, 2 , Yu Zuo 1 , Srilakshmi Yalavarthi 1 , Kelsey Gockman 1 , Melanie Zuo 3 , Jacqueline A Madison 1 , Christopher Blair 4 , Wrenn Woodward 5 , Sean P Lezak 5 , Njira L Lugogo 6 , Robert J Woods 4 , Christian Lood 7 , Jason S Knight 1 , Yogendra Kanthi 8, 9
Journal of Leukocyte Biology ( IF 3.6 ) Pub Date : 2020-09-01 , DOI: 10.1002/jlb.3covcra0720-359r Hui Shi 1, 2 , Yu Zuo 1 , Srilakshmi Yalavarthi 1 , Kelsey Gockman 1 , Melanie Zuo 3 , Jacqueline A Madison 1 , Christopher Blair 4 , Wrenn Woodward 5 , Sean P Lezak 5 , Njira L Lugogo 6 , Robert J Woods 4 , Christian Lood 7 , Jason S Knight 1 , Yogendra Kanthi 8, 9
Affiliation
|
Severe cases of coronavirus disease 2019 (COVID‐19) are regularly complicated by respiratory failure. Although it has been suggested that elevated levels of blood neutrophils associate with worsening oxygenation in COVID‐19, it is unknown whether neutrophils are drivers of the thrombo‐inflammatory storm or simple bystanders. To better understand the potential role of neutrophils in COVID‐19, we measured levels of the neutrophil activation marker S100A8/A9 (calprotectin) in hospitalized patients and determined its relationship to severity of illness and respiratory status. Patients with COVID‐19 (n = 172) had markedly elevated levels of calprotectin in their blood. Calprotectin tracked with other acute phase reactants including C‐reactive protein, ferritin, lactate dehydrogenase, and absolute neutrophil count, but was superior in identifying patients requiring mechanical ventilation. In longitudinal samples, calprotectin rose as oxygenation worsened. When tested on day 1 or 2 of hospitalization (n = 94 patients), calprotectin levels were significantly higher in patients who progressed to severe COVID‐19 requiring mechanical ventilation (8039 ± 7031 ng/ml, n = 32) as compared to those who remained free of intubation (3365 ± 3146, P < 0.0001). In summary, serum calprotectin levels track closely with current and future COVID‐19 severity, implicating neutrophils as potential perpetuators of inflammation and respiratory compromise in COVID‐19.
中文翻译:

中性粒细胞钙卫蛋白可识别 COVID-19 中的严重肺部疾病。
严重的 2019 年冠状病毒病 (COVID-19) 病例经常并发呼吸衰竭。尽管有人提出血液中性粒细胞水平升高与 COVID-19 氧合恶化有关,但尚不清楚中性粒细胞是血栓炎症风暴的驱动因素还是简单的旁观者。为了更好地了解中性粒细胞在 COVID-19 中的潜在作用,我们测量了住院患者中中性粒细胞激活标志物 S100A8/A9(钙卫蛋白)的水平,并确定了其与疾病严重程度和呼吸状态的关系。COVID-19 患者(n = 172) 血液中的钙卫蛋白水平显着升高。钙卫蛋白与其他急性期反应物(包括 C 反应蛋白、铁蛋白、乳酸脱氢酶和绝对中性粒细胞计数)一起追踪,但在识别需要机械通气的患者方面具有优势。在纵向样本中,钙卫蛋白随着氧合恶化而上升。在住院的第 1 天或第 2 天进行测试时(n = 94 名患者),与需要机械通气的严重 COVID-19 患者相比,钙卫蛋白水平显着更高(8039 ± 7031 ng/ml,n = 32)。仍然没有插管 (3365 ± 3146, P < 0.0001)。总之,血清钙卫蛋白水平与当前和未来的 COVID-19 严重程度密切相关,表明中性粒细胞是 COVID-19 炎症和呼吸系统损害的潜在持续因素。
更新日期:2020-09-01
中文翻译:

中性粒细胞钙卫蛋白可识别 COVID-19 中的严重肺部疾病。
严重的 2019 年冠状病毒病 (COVID-19) 病例经常并发呼吸衰竭。尽管有人提出血液中性粒细胞水平升高与 COVID-19 氧合恶化有关,但尚不清楚中性粒细胞是血栓炎症风暴的驱动因素还是简单的旁观者。为了更好地了解中性粒细胞在 COVID-19 中的潜在作用,我们测量了住院患者中中性粒细胞激活标志物 S100A8/A9(钙卫蛋白)的水平,并确定了其与疾病严重程度和呼吸状态的关系。COVID-19 患者(n = 172) 血液中的钙卫蛋白水平显着升高。钙卫蛋白与其他急性期反应物(包括 C 反应蛋白、铁蛋白、乳酸脱氢酶和绝对中性粒细胞计数)一起追踪,但在识别需要机械通气的患者方面具有优势。在纵向样本中,钙卫蛋白随着氧合恶化而上升。在住院的第 1 天或第 2 天进行测试时(n = 94 名患者),与需要机械通气的严重 COVID-19 患者相比,钙卫蛋白水平显着更高(8039 ± 7031 ng/ml,n = 32)。仍然没有插管 (3365 ± 3146, P < 0.0001)。总之,血清钙卫蛋白水平与当前和未来的 COVID-19 严重程度密切相关,表明中性粒细胞是 COVID-19 炎症和呼吸系统损害的潜在持续因素。

































 京公网安备 11010802027423号
京公网安备 11010802027423号