当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Drug-Coated Balloon Angioplasty Versus Drug-Eluting Stent Implantation in Patients With Coronary Stent Restenosis
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2020-06-01 , DOI: 10.1016/j.jacc.2020.04.006 Daniele Giacoppo 1 , Fernando Alfonso 2 , Bo Xu 3 , Bimmer E P M Claessen 4 , Tom Adriaenssens 5 , Christoph Jensen 6 , María J Pérez-Vizcayno 7 , Do-Yoon Kang 8 , Ralf Degenhardt 9 , Leos Pleva 10 , Jan Baan 11 , Javier Cuesta 2 , Duk-Woo Park 8 , Pavel Kukla 10 , Pilar Jiménez-Quevedo 7 , Martin Unverdorben 12 , Runlin Gao 3 , Christoph K Naber 6 , Seung-Jung Park 8 , José P S Henriques 11 , Adnan Kastrati 13 , Robert A Byrne 14
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2020-06-01 , DOI: 10.1016/j.jacc.2020.04.006 Daniele Giacoppo 1 , Fernando Alfonso 2 , Bo Xu 3 , Bimmer E P M Claessen 4 , Tom Adriaenssens 5 , Christoph Jensen 6 , María J Pérez-Vizcayno 7 , Do-Yoon Kang 8 , Ralf Degenhardt 9 , Leos Pleva 10 , Jan Baan 11 , Javier Cuesta 2 , Duk-Woo Park 8 , Pavel Kukla 10 , Pilar Jiménez-Quevedo 7 , Martin Unverdorben 12 , Runlin Gao 3 , Christoph K Naber 6 , Seung-Jung Park 8 , José P S Henriques 11 , Adnan Kastrati 13 , Robert A Byrne 14
Affiliation
|
BACKGROUND
In patients with coronary in-stent restenosis (ISR) requiring reintervention, it is unclear if the choice of treatment should depend on whether the restenotic stent was a bare-metal stent (BMS) or a drug-eluting stent (DES). OBJECTIVES
This study aimed to assess the comparative efficacy and safety of the 2 most frequently used treatments - angioplasty with drug-coated balloon (DCB) and repeat stenting DES - in patients with BMS-and DES-ISR. METHODS
The DAEDALUS (Difference in Antirestenotic Effectiveness of Drug-Eluting Stent and Drug-Coated Balloon Angioplasty for the Occurrence of Coronary In-Stent Restenosis) study was a pooled analysis of individual patient data from all 10 existing randomized clinical trials comparing DCB angioplasty with repeat DES implantation for the treatment of coronary ISR. In this pre-specified analysis, patients were stratified according to BMS- versus DES-ISR and treatment assigned. The primary efficacy endpoint was target lesion revascularization (TLR) at 3 years. The primary safety endpoint was a composite of all-cause death, myocardial infarction, or target lesion thrombosis at 3 years. Primary analysis was performed by mixed-effects Cox models accounting for the trial of origin. Secondary analyses included nonparsimonious multivariable adjustment accounting also for multiple lesions per patient and 2-stage analyses. RESULTS
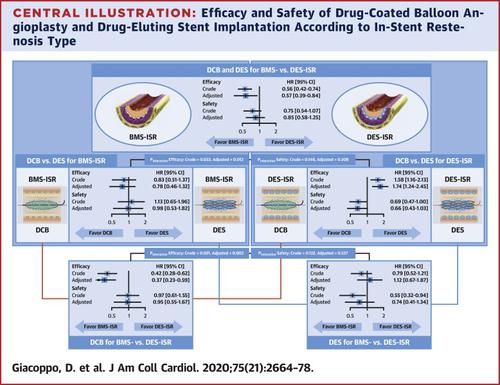
A total of 710 patients with BMS-ISR (722 lesions) and 1,248 with DES-ISR (1,377 lesions) were included. In patients with BMS-ISR, no significant difference between treatments was observed in terms of primary efficacy (9.2% vs. 10.2%; hazard ratio [HR]: 0.83; 95% confidence interval [CI]: 0.51 to 1.37) and safety endpoints (8.7% vs. 7.5%; HR: 1.13; 95% CI: 0.65 to 1.96); results of secondary analyses were consistent. In patients with DES-ISR, the risk of the primary efficacy endpoint was higher with DCB angioplasty than with repeat DES implantation (20.3% vs. 13.4%; HR: 1.58; 95% CI: 1.16 to 2.13), whereas the risk of the primary safety endpoint was numerically lower (9.5% vs. 13.3%; HR: 0.69; 95% CI: 0.47 to 1.00); results of secondary analyses were consistent. Regardless of the treatment used, the risk of TLR was lower in BMS- versus DES-ISR (9.7% vs. 17.0%; HR: 0.56; 95% CI: 0.42 to 0.74), whereas safety was not significantly different between ISR types. CONCLUSIONS
At 3-year follow-up, DCB angioplasty and repeat stenting with DES are similarly effective and safe in the treatment of BMS-ISR, whereas DCB angioplasty is significantly less effective than repeat DES implantation in the treatment DES-ISR, and associated with a nonsignificant reduction in the primary composite safety endpoint. Overall, DES-ISR is associated with higher rates of treatment failure and similar safety compared with BMS-ISR.
中文翻译:

冠状动脉支架再狭窄患者药物涂层球囊血管成形术与药物洗脱支架植入术的比较
背景 在需要再次干预的冠状动脉支架内再狭窄 (ISR) 患者中,尚不清楚治疗的选择是否应取决于再狭窄支架是裸金属支架 (BMS) 还是药物洗脱支架 (DES)。目的 本研究旨在评估 BMS 和 DES-ISR 患者最常用的 2 种治疗方法 - 药物涂层球囊 (DCB) 血管成形术和重复支架置入术 DES 的比较疗效和安全性。方法 DAEDALUS (药物洗脱支架和药物涂层球囊血管成形术对冠状动脉支架内再狭窄发生抗再狭窄效果的差异) 研究是对来自所有 10 项现有随机临床试验的个体患者数据的汇总分析,比较 DCB 血管成形术与重复 DES 植入治疗冠状动脉 ISR。在这项预先指定的分析中,根据 BMS 与 DES-ISR 和分配的治疗对患者进行分层。主要疗效终点是 3 年时的靶病变血运重建 (TLR)。主要安全性终点是 3 年时全因死亡、心肌梗死或靶病变血栓形成的复合终点。通过考虑原始试验的混合效应 Cox 模型进行初步分析。二次分析包括非简约多变量调整,也考虑了每位患者的多个病灶和 2 阶段分析。结果 共纳入 710 例 BMS-ISR 患者 (722 个病灶) 和 1,248 例 DES-ISR 患者 (1,377 个病灶)。在 BMS-ISR 患者中,在主要疗效 (9.2% vs. 10.2%;风险比 [HR]: 0.83;95% 置信区间 [CI]: 0.51 至 1.37) 和安全终点 (8.7% vs. 7.5%;心率:1.13;95% CI:0.65 至 1。96);二次分析的结果一致。在 DES-ISR 患者中,DCB 血管成形术的主要疗效终点风险高于重复 DES 植入 (20.3% vs. 13.4%;心率:1.58;95% CI:1.16 至 2.13),而主要安全终点的风险在数值上较低(9.5% 对 13.3%;心率:0.69;95% CI:0.47 至 1.00);二次分析的结果一致。无论使用何种治疗方法,BMS 与 DES-ISR 的 TLR 风险较低(9.7% 对 17.0%;心率:0.56;95% CI:0.42 至 0.74),而 ISR 类型之间的安全性没有显著差异。结论在 3 年随访中,DCB 血管成形术和重复支架置入术治疗 BMS-ISR 同样有效和安全,而 DCB 血管成形术在治疗 DES-ISR 时明显不如重复植入 DES 有效,并且与主要复合安全终点的不显着降低相关。总体而言,与 BMS-ISR 相比,DES-ISR 与更高的治疗失败率和相似的安全性相关。
更新日期:2020-06-01
中文翻译:

冠状动脉支架再狭窄患者药物涂层球囊血管成形术与药物洗脱支架植入术的比较
背景 在需要再次干预的冠状动脉支架内再狭窄 (ISR) 患者中,尚不清楚治疗的选择是否应取决于再狭窄支架是裸金属支架 (BMS) 还是药物洗脱支架 (DES)。目的 本研究旨在评估 BMS 和 DES-ISR 患者最常用的 2 种治疗方法 - 药物涂层球囊 (DCB) 血管成形术和重复支架置入术 DES 的比较疗效和安全性。方法 DAEDALUS (药物洗脱支架和药物涂层球囊血管成形术对冠状动脉支架内再狭窄发生抗再狭窄效果的差异) 研究是对来自所有 10 项现有随机临床试验的个体患者数据的汇总分析,比较 DCB 血管成形术与重复 DES 植入治疗冠状动脉 ISR。在这项预先指定的分析中,根据 BMS 与 DES-ISR 和分配的治疗对患者进行分层。主要疗效终点是 3 年时的靶病变血运重建 (TLR)。主要安全性终点是 3 年时全因死亡、心肌梗死或靶病变血栓形成的复合终点。通过考虑原始试验的混合效应 Cox 模型进行初步分析。二次分析包括非简约多变量调整,也考虑了每位患者的多个病灶和 2 阶段分析。结果 共纳入 710 例 BMS-ISR 患者 (722 个病灶) 和 1,248 例 DES-ISR 患者 (1,377 个病灶)。在 BMS-ISR 患者中,在主要疗效 (9.2% vs. 10.2%;风险比 [HR]: 0.83;95% 置信区间 [CI]: 0.51 至 1.37) 和安全终点 (8.7% vs. 7.5%;心率:1.13;95% CI:0.65 至 1。96);二次分析的结果一致。在 DES-ISR 患者中,DCB 血管成形术的主要疗效终点风险高于重复 DES 植入 (20.3% vs. 13.4%;心率:1.58;95% CI:1.16 至 2.13),而主要安全终点的风险在数值上较低(9.5% 对 13.3%;心率:0.69;95% CI:0.47 至 1.00);二次分析的结果一致。无论使用何种治疗方法,BMS 与 DES-ISR 的 TLR 风险较低(9.7% 对 17.0%;心率:0.56;95% CI:0.42 至 0.74),而 ISR 类型之间的安全性没有显著差异。结论在 3 年随访中,DCB 血管成形术和重复支架置入术治疗 BMS-ISR 同样有效和安全,而 DCB 血管成形术在治疗 DES-ISR 时明显不如重复植入 DES 有效,并且与主要复合安全终点的不显着降低相关。总体而言,与 BMS-ISR 相比,DES-ISR 与更高的治疗失败率和相似的安全性相关。































 京公网安备 11010802027423号
京公网安备 11010802027423号