EuroIntervention ( IF 7.6 ) Pub Date : 2021-06-11 , DOI: 10.4244/eij-d-19-00997 Jana Vavrova 1 , Boris Koznar , Tomas Peisker , Peter Vasko , Filip Rohac , Jakub Sulzenko , Josef Kroupa , Ivana Stetkarova , Luca Mengozzi , Marek Petras , Petr Widimsky
Background: Thrombectomy is an effective treatment for acute ischaemic stroke (AIS).
Aims: The aim of this study was to compare clinical outcomes with intracranial artery occlusion site among AIS patients treated in the setting of a cardiology cath lab.
Methods: This was a single-centre, prospective registry of 214 consecutive patients with AIS enrolled between 2012 and 2018. All thrombectomy procedures were performed in a cardiology cath lab with stent retrievers or aspiration systems. The functional outcome was assessed by the modified Rankin Scale (mRS) after three months.
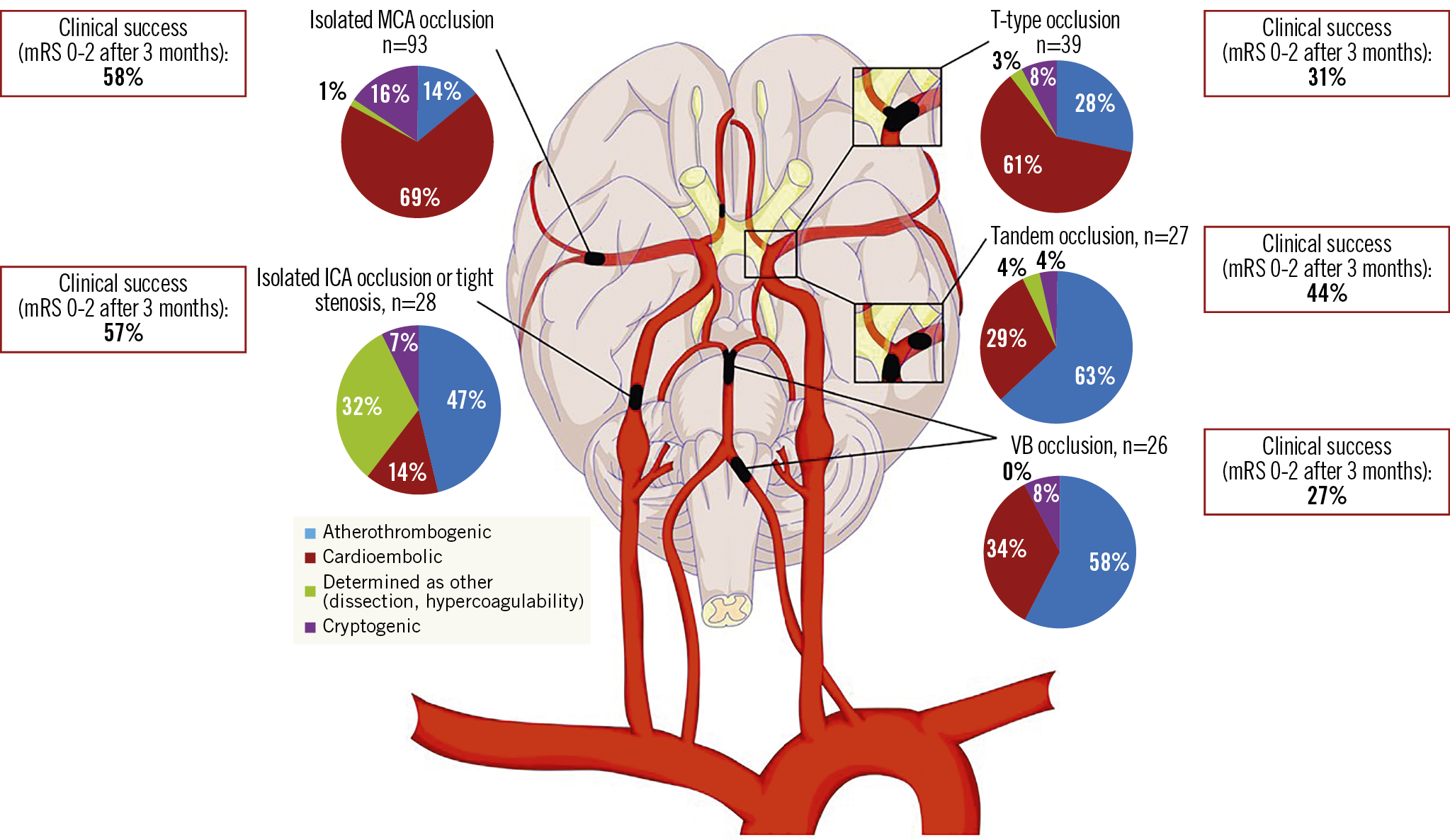
Results: Ninety-three patients (44%) had middle cerebral artery (MCA) occlusion, 28 patients (13%) had proximal internal carotid artery (ICA) occlusion, 27 patients (13%) had tandem (ICA+MCA) occlusion, 39 patients (18%) had terminal ICA (T-type) occlusion, and 26 patients (12%) had vertebrobasilar (VB) stroke. Favourable clinical outcome (mRS ≤2) was reached in 58% of MCA occlusions and in 56% of isolated ICA occlusions, but in only 31% of T-type occlusions and in 27% of VB stroke. Poor clinical outcome in T-type occlusions and VB strokes was influenced by the lower recanalisation success (mTICI 2b-3 flow) rates: 56% (T-type) and 50% (VB) compared to 82% in MCA occlusions, 89% in isolated ICA occlusions and 96% in tandem occlusions.
Conclusions: Catheter-based thrombectomy achieved significantly better clinical results in patients with isolated MCA occlusion, isolated ICA occlusions or tight stenosis and tandem occlusions compared to patients with T-type occlusion and posterior strokes.
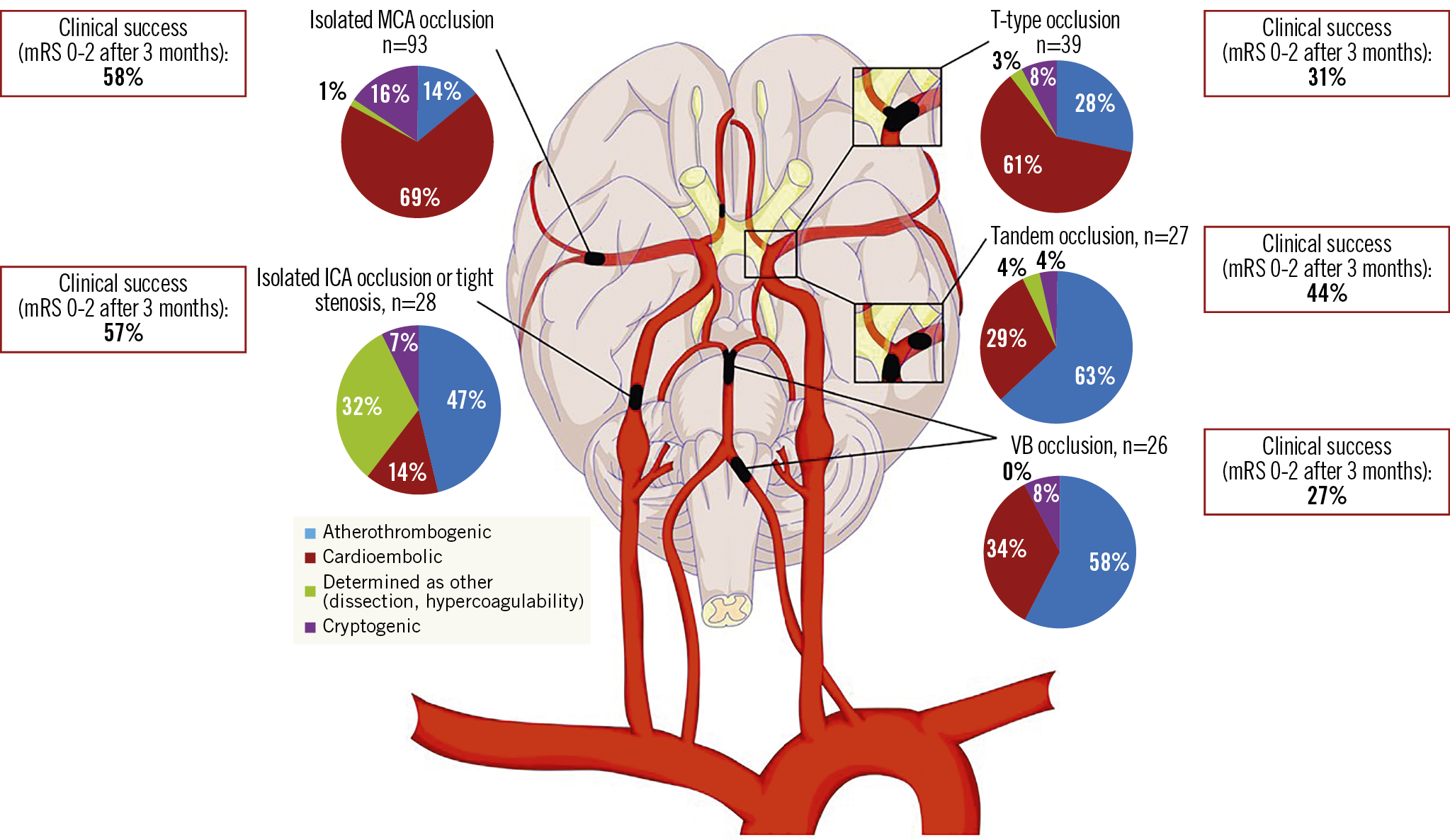
Visual summary. Endovascular intervention of isolated MCA or ICA occlusions provides greatest clinical benefit, while interventions in posterior circulation have lower chance for clinical success.
中文翻译:

动脉闭塞和卒中病因对急性缺血性卒中进行血栓切除术的长期结果:一项 PRAGUE-16 子研究
背景:血栓切除术是治疗急性缺血性卒中 (AIS) 的有效方法。
目的:本研究的目的是比较在心脏病导管室接受治疗的 AIS 患者中颅内动脉闭塞部位的临床结果。
方法:这是一项单中心、前瞻性登记,纳入了 2012 年至 2018 年间连续入组的 214 名 AIS 患者。所有取栓手术均在心脏病导管室进行,配备支架取栓器或抽吸系统。三个月后通过改良 Rankin 量表 (mRS) 评估功能结果。
结果: 93 例 (44%) 有大脑中动脉 (MCA) 闭塞,28 例 (13%) 有近端颈内动脉 (ICA) 闭塞,27 例 (13%) 有串联 (ICA+MCA) 闭塞, 39 名患者 (18%) 患有终末 ICA(T 型)闭塞,26 名患者 (12%) 患有椎基底动脉 (VB) 卒中。58% 的 MCA 闭塞和 56% 的单独 ICA 闭塞达到了良好的临床结果 (mRS ≤2),但只有 31% 的 T 型闭塞和 27% 的 VB 卒中。T 型闭塞和 VB 中风的不良临床结果受到较低再通成功率(mTICI 2b-3 流量)的影响:56%(T 型)和 50%(VB),而 MCA 闭塞为 82%,89%在孤立的 ICA 闭塞和 96% 的串联闭塞中。
结论:与 T 型闭塞和后部卒中患者相比,基于导管的血栓切除术在孤立性 MCA 闭塞、孤立性 ICA 闭塞或紧密狭窄和串联闭塞患者中取得了显着更好的临床效果。
视觉总结。孤立性 MCA 或 ICA 闭塞的血管内介入治疗可提供最大的临床益处,而后循环介入治疗获得临床成功的机会较低。

































 京公网安备 11010802027423号
京公网安备 11010802027423号