当前位置:
X-MOL 学术
›
Eur. J. Heart Fail.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Timing of veno‐arterial extracorporeal membrane oxygenation support in patients with cardiogenic shock
European Journal of Heart Failure ( IF 16.9 ) Pub Date : 2024-10-24 , DOI: 10.1002/ejhf.3498 Jonas Sundermeyer, Caroline Kellner, Benedikt N. Beer, Angela Dettling, Lisa Besch, Stefan Blankenberg, Ingo Eitel, Derk Frank, Norbert Frey, Tobias Graf, Paulus Kirchhof, Jannis Krais, Dirk von Lewinski, Norman Mangner, Sven Möbius‐Winkler, Peter Nordbeck, Martin Orban, Matthias Pauschinger, Can Martin Sag, Clemens Scherer, Carsten Skurk, Holger Thiele, Dirk Westermann, Benedikt Schrage
European Journal of Heart Failure ( IF 16.9 ) Pub Date : 2024-10-24 , DOI: 10.1002/ejhf.3498 Jonas Sundermeyer, Caroline Kellner, Benedikt N. Beer, Angela Dettling, Lisa Besch, Stefan Blankenberg, Ingo Eitel, Derk Frank, Norbert Frey, Tobias Graf, Paulus Kirchhof, Jannis Krais, Dirk von Lewinski, Norman Mangner, Sven Möbius‐Winkler, Peter Nordbeck, Martin Orban, Matthias Pauschinger, Can Martin Sag, Clemens Scherer, Carsten Skurk, Holger Thiele, Dirk Westermann, Benedikt Schrage
|
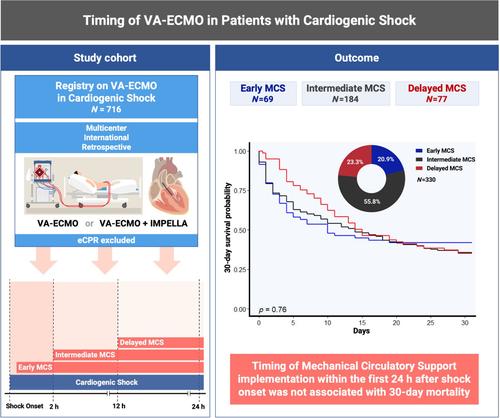
AimsThe optimal timing for implementing mechanical circulatory support (MCS) in cardiogenic shock (CS) remains indeterminate. This study aims to evaluate patient characteristics and outcome associated with the time interval between CS onset and veno‐arterial extracorporeal membrane oxygenation (VA‐ECMO) implementation.Methods and resultsIn this study, patients with CS treated with MCS at 15 tertiary care centres in three countries were enrolled. Patients treated with MCS were stratified into early (<2 h), intermediate (2–12 h) and delayed (≥12–24 h) MCS implantation by using the time interval between CS onset and MCS device implementation. Adjusted logistic and Cox regression models were fitted to assess the association between timing of MCS implementation, patient characteristics and 30‐day mortality. A total of 330 patients with CS treated with VA‐ECMO and/or microaxial flow pump were included in this study; 20.9% received early, 55.8% intermediate, and 23.3% delayed MCS. Although crude 30‐day mortality was slightly lower in patients with early MCS (58.1% vs. 64.7% vs. 64.3%), adjusted analyses showed no significant association between timing of MCS implantation and 30‐day all‐cause mortality (hazard ratio [HR] for early vs. intermediate MCS: 0.93, 95% confidence interval [CI] 0.59–1.46, p = 0.74; HR for early vs. delayed MCS: 1.29, 95% CI 0.78–2.13, p = 0.33). Moreover, the incidence of complications, related and unrelated to MCS, did not differ significantly among groups.ConclusionIn this exploratory study of patients with CS treated with MCS, the timing of device implantation within 24 h after CS onset was not associated with mortality. This supports a restrictive MCS approach, reserving its application for patients experiencing CS deterioration despite conventional therapy.
中文翻译:

心源性休克患者静脉-动脉体外膜肺氧合支持的时机
目的在心源性休克 (CS) 中实施机械循环支持 (MCS) 的最佳时间仍不确定。本研究旨在评估与 CS 发作和静脉-动脉体外膜肺氧合 (VA-ECMO) 实施之间的时间间隔相关的患者特征和结果。方法和结果在本研究中,在 3 个国家的 15 个三级医疗中心接受了 MCS 治疗的 CS 患者被纳入。使用 CS 发作和 MCS 装置实施之间的时间间隔,将接受 MCS 治疗的患者分为早期 (<2 h)、中期 (2-12 h) 和延迟 (≥12-24 h) MCS 植入。拟合调整后的 logistic 和 Cox 回归模型,以评估 MCS 实施时间、患者特征和 30 天死亡率之间的关联。本研究共纳入 330 例接受 VA-ECMO 和/或微轴流泵治疗的 CS 患者;20.9% 接受早期 MCS,55.8% 接受中期 MCS,23.3% 延迟接受 MCS。尽管早期 MCS 患者的粗 30 天死亡率略低(58.1% 对 64.7% 对 64.3%),但调整后的分析显示 MCS 植入时间与 30 天全因死亡率之间没有显著关联(早期与中期 MCS 的风险比 [HR]:0.93,95% 置信区间 [CI] 0.59-1.46,p = 0.74;早期与延迟 MCS 的 HR:1.29,95% CI 0.78-2.13,p = 0.33)。此外,与 MCS 相关和无关的并发症的发生率在组间没有显著差异。结论在这项针对 MCS 治疗的 CS 患者的探索性研究中,CS 发作后 24 小时内装置植入的时间与死亡率无关。 这支持限制性 MCS 方法,将其应用于尽管接受常规治疗但仍出现 CS 恶化的患者。
更新日期:2024-10-24
中文翻译:

心源性休克患者静脉-动脉体外膜肺氧合支持的时机
目的在心源性休克 (CS) 中实施机械循环支持 (MCS) 的最佳时间仍不确定。本研究旨在评估与 CS 发作和静脉-动脉体外膜肺氧合 (VA-ECMO) 实施之间的时间间隔相关的患者特征和结果。方法和结果在本研究中,在 3 个国家的 15 个三级医疗中心接受了 MCS 治疗的 CS 患者被纳入。使用 CS 发作和 MCS 装置实施之间的时间间隔,将接受 MCS 治疗的患者分为早期 (<2 h)、中期 (2-12 h) 和延迟 (≥12-24 h) MCS 植入。拟合调整后的 logistic 和 Cox 回归模型,以评估 MCS 实施时间、患者特征和 30 天死亡率之间的关联。本研究共纳入 330 例接受 VA-ECMO 和/或微轴流泵治疗的 CS 患者;20.9% 接受早期 MCS,55.8% 接受中期 MCS,23.3% 延迟接受 MCS。尽管早期 MCS 患者的粗 30 天死亡率略低(58.1% 对 64.7% 对 64.3%),但调整后的分析显示 MCS 植入时间与 30 天全因死亡率之间没有显著关联(早期与中期 MCS 的风险比 [HR]:0.93,95% 置信区间 [CI] 0.59-1.46,p = 0.74;早期与延迟 MCS 的 HR:1.29,95% CI 0.78-2.13,p = 0.33)。此外,与 MCS 相关和无关的并发症的发生率在组间没有显著差异。结论在这项针对 MCS 治疗的 CS 患者的探索性研究中,CS 发作后 24 小时内装置植入的时间与死亡率无关。 这支持限制性 MCS 方法,将其应用于尽管接受常规治疗但仍出现 CS 恶化的患者。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号