Diabetologia ( IF 8.4 ) Pub Date : 2024-10-03 , DOI: 10.1007/s00125-024-06281-7 Andrew Cole, Nicholas Weight, Shivani Mishra, Julia Grapsa, Martin K. Rutter, Zbigniew Siudak, Saadiq Moledina, Evangelos Kontopantelis, Kamlesh Khunti, Mamas A. Mamas
|
Aims/hypothesis
The aim of this study was to investigate how diabetes mellitus affects longer term outcomes in individuals presenting to hospital with non-ST segment elevation myocardial infarction (NSTEMI).
Methods
We analysed data from 456,376 adults hospitalised between January 2005 and March 2019 with NSTEMI from the UK Myocardial Ischaemia National Audit Project (MINAP) registry, linked with Office for National Statistics death reporting. We compared outcomes and quality of care by diabetes status.
Results
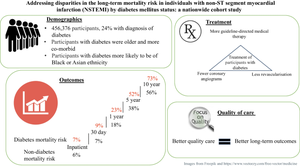
Individuals with diabetes were older (median age 74 vs 73 years), were more often of Asian ethnicity (13% vs 4%) and underwent revascularisation (percutaneous coronary intervention or coronary artery bypass graft surgery) (38% vs 40%) less frequently than those without diabetes. The mortality risk for those with diabetes compared with those without was significantly higher at 30 days (HR 1.19, 95% CI 1.15, 1.23), 1 year (HR 1.28, 95% CI 1.26, 1.31), 5 years (HR 1.36, 95% CI 1.34, 1.38) and 10 years (HR 1.39, 95% CI 1.36, 1.42). In individuals with diabetes, higher quality inpatient care, assessed by opportunity-based quality indicator (OBQI) score category (‘poor’, ‘fair’, ‘good’ or ‘excellent’), was associated with lower mortality rates compared with poor care (good: HR 0.74, 95% CI 0.73, 0.76; excellent: HR 0.69, 95% CI 0.68, 0.71). In addition, compared with poor care, excellent care in the diabetes group was associated with the lowest mortality rates in the diet-treated and insulin-treated subgroups (diet-treated: HR 0.64, 95% CI 0.61, 0.68; insulin-treated: HR 0.69, CI 0.66, 0.72).
Conclusion/interpretation
Individuals with diabetes experience disparities during inpatient care following NSTEMI. They have a higher risk of long-term mortality than those without diabetes, and higher quality inpatient care may lead to better long-term survival.
Graphical Abstract
中文翻译:

解决糖尿病状态导致非 ST 段心肌梗死 (NSTEMI) 个体长期死亡风险的差异:一项全国性队列研究
目标/假设
本研究的目的是调查糖尿病如何影响因非 ST 段抬高型心肌梗死 (NSTEMI) 住院的个体的长期结局。
方法
我们分析了 2005 年 1 月至 2019 年 3 月期间因 NSTEMI 住院的 456,376 名成年人的数据,这些数据来自英国心肌缺血国家审计项目 (MINAP) 登记处,与国家统计局死亡报告相关联。我们按糖尿病状况比较了结局和护理质量。
结果
与非糖尿病患者相比,糖尿病患者年龄较大(中位年龄为 74 岁对 73 岁),亚裔更常见(13% 对 4%),并且接受血运重建(经皮冠状动脉介入治疗或冠状动脉旁路移植手术)(38% 对 40%)的频率较低。与非糖尿病患者相比,糖尿病患者的死亡风险在 30 天 (HR 1.19, 95% CI 1.15, 1.23) 、1 年 (HR 1.28, 95% CI 1.26, 1.31)、5 年 (HR 1.36, 95% CI 1.34, 1.38) 和 10 年 (HR 1.39, 95% CI 1.36, 1.42) 时显著升高。在糖尿病患者中,与护理不佳相比,通过基于机会的质量指标 (OBQI) 评分类别(“差”、“一般”、“好”或“优秀”)评估的更高质量的住院护理与较低的死亡率相关(良好:HR 0.74,95% CI 0.73,0.76;优秀:HR 0.69,95% CI 0.68,0.71)。此外,与不良护理相比,糖尿病组的良好护理与饮食治疗和胰岛素治疗亚组中最低的死亡率相关(饮食治疗:HR 0.64,95% CI 0.61,0.68;胰岛素治疗:HR 0.69,CI 0.66,0.72)。
结论/解释
糖尿病患者在 NSTEMI 后的住院护理期间经历差异。与非糖尿病患者相比,他们的长期死亡风险更高,更高质量的住院护理可能会带来更好的长期生存率。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号