Diabetologia ( IF 8.4 ) Pub Date : 2024-09-13 , DOI: 10.1007/s00125-024-06273-7 Astrid Lavens 1 , Christophe De Block 2 , Philippe Oriot 3 , Laurent Crenier 4 , Jean-Christophe Philips 5 , Michel Vandenbroucke 6 , An-Sofie Vanherwegen 1 , Frank Nobels 7 , Chantal Mathieu 8 ,
|
Aims/hypothesis
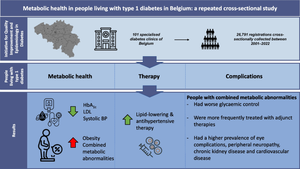
Metabolic abnormalities such as central obesity, insulin resistance, dyslipidaemia and hypertension, often referred to as ‘the metabolic syndrome’ (or ‘combined metabolic abnormalities’), are increasingly being identified in people living with type 1 diabetes, accelerating the risk for CVD. As a result, in recent years, treatment in people living with type 1 diabetes has shifted to improving overall metabolic health rather than glucose control alone. In Belgium, diabetes care for people living with type 1 diabetes is centrally organised. The Initiative for Quality Improvement and Epidemiology in Diabetes, imposed by the Belgian health insurance system, has systematically collected data from patients on intensive insulin therapy treated in all 101 diabetes clinics in Belgium since 2001. The aim of this real-world study is to describe the evolution of treatment and metabolic health, including the prevalence of obesity and combined metabolic abnormalities, in people living with type 1 diabetes over the past 20 years, and to compare the treatment and prevalence of complications between those with and without combined metabolic abnormalities.
Methods
We analysed data on adults (≥16 years old) living with type 1 diabetes, who were diagnosed at age ≤45 years and who had a diabetes duration ≥1 year, collected between 2001 and 2022. The evolution of HbA1c, BMI, LDL-cholesterol, systolic BP, lipid-lowering therapy and antihypertensive therapy over time was analysed. The prevalence of individual and multiple metabolic abnormalities according to various definitions of the metabolic syndrome/combined metabolic abnormalities was analysed, and the association between combined metabolic abnormalities and metabolic health indicators, complications and treatment was investigated in the 2022 data.
Results
The final dataset consisted of 26,791 registrations of adults living with type 1 diabetes collected between 2001 and 2022. Although glycaemic and lipid control generally improved over time, the prevalence of obesity strongly increased (12.1% in 2001 vs 21.7% in 2022, p<0.0001), as did the presence of combined metabolic abnormalities (WHO criteria: 26.9% in 2001 vs 42.9% in 2022 in women, p<0.0001; 30.4% in 2001 vs 52.1% in 2022 in men, p<0.0001; WHO criteria without albuminuria: 22.3% in 2001 vs 40.6% in 2022 in women, p<0.0001; 25.1% in 2001 vs 49.2% in 2022 in men, p<0.0001; NCEP-ATPIII criteria: 39.9% in 2005 vs 57.2% in 2022 in women, p<0.0001; 40.8% in 2005 vs 60.9% in 2022 in men, p<0.0001; IDF criteria: 43.9% in 2005 vs 59.3% in 2022 in women, p<0.001; 33.7% in 2005 vs 50.0% in 2022 in men, p<0.0001). People with combined metabolic abnormalities had higher glucose levels compared to those without combined metabolic abnormalities (HbA1c >58 mmol in men: 48.9% vs 36.9%; HbA1c >58 mmol in women: 53.3% vs 41.1%, p<0.0001). People with combined metabolic abnormalities were more often treated with adjunct therapies such as metformin, sodium–glucose transport protein 2 inhibitors and glucagon-like peptide-1 receptor agonists. In both men and women, the presence of combined metabolic abnormalities was strongly related to the presence of eye complications, peripheral neuropathy, chronic kidney disease and CVD, corrected for age, diabetes duration and HbA1c.
Conclusions/interpretation
Overweight, obesity and combined metabolic abnormalities are increasingly being identified in people living with type 1 diabetes, further accelerating the risk of microvascular and macrovascular complications. Early identification of the presence of combined metabolic abnormalities should enable therapeutic interventions to be modified towards multifactorial approaches, with attention to education on avoidance of overweight (e.g. dietary counselling) in addition to strict glycaemic control and intensification of use of antihypertensive agents and statins. Use of adjunct therapies in this population as a tool should be explored more thoroughly to reduce risk of complications.
Graphical Abstract
中文翻译:

比利时 1 型糖尿病患者的代谢健康:一项重复横断面研究
目标/假设
中心性肥胖、胰岛素抵抗、血脂异常和高血压等代谢异常,通常被称为“代谢综合征”(或“联合代谢异常”),越来越多地在 1 型糖尿病患者中被发现,从而增加了 CVD 的风险。因此,近年来,1 型糖尿病患者的治疗已转向改善整体代谢健康,而不仅仅是控制血糖。在比利时,1 型糖尿病患者的糖尿病护理是集中组织的。比利时健康保险系统实施的糖尿病质量改进和流行病学倡议,系统地收集了自 2001 年以来在比利时所有 101 家糖尿病诊所接受强化胰岛素治疗的患者的数据。这项现实世界研究的目的是描述过去 20 年来 1 型糖尿病患者治疗和代谢健康的演变,包括肥胖和合并代谢异常的患病率,并比较患有和不患有合并代谢异常的患者之间的治疗和并发症患病率。
方法
我们分析了 2001 年至 2022 年间收集的患有 1 型糖尿病的成年人(≥16 岁)的数据,这些患者的诊断年龄≤45 岁且糖尿病病程≥1 年。HbA 1c 、BMI、LDL 的演变-分析随时间推移的胆固醇、收缩压、降脂治疗和抗高血压治疗。根据代谢综合征/组合代谢异常的不同定义,分析了个体和多种代谢异常的患病率,并在2022年的数据中调查了组合代谢异常与代谢健康指标、并发症和治疗之间的关联。
结果
最终数据集包含 2001 年至 2022 年间收集的 26,791 名患有 1 型糖尿病的成年人的登记。尽管随着时间的推移,血糖和血脂控制普遍有所改善,但肥胖患病率大幅增加(2001 年为 12.1%,2022 年为 21.7%, p <0 .0001),以及合并代谢异常的存在(世界卫生组织标准:2001 年女性为 26.9%,2022 年为 42.9%, p <0.0001;男性为 2001 年 30.4%,2022 年为 52.1%, p <0.0001)。 0001;世界卫生组织无蛋白尿标准:2001 年女性为 22.3%,2022 年为 40.6%, p <0.0001;2001 年为 25.1%,2022 年男性为 49.2%, p <0.0001; 2005 年女性为 57.2%, p <0.0001;2005 年男性为 40.8%,2022 年为 60.9%, p <0.0001;IDF 标准:2005 年女性为 43.9%,2022 年为 59.3%, p <0.001;2005 年男性为 33.7%,2022 年为 50.0%, p <0.0001)。与没有合并代谢异常的人相比,合并代谢异常的人的血糖水平较高(男性 HbA 1c >58 mmol:48.9% vs 36.9%;女性 HbA 1c >58 mmol:53.3% vs 41.1%, p <0.0001 )。合并代谢异常的患者更常接受辅助治疗,例如二甲双胍、钠-葡萄糖转运蛋白 2 抑制剂和胰高血糖素样肽 1 受体激动剂。在男性和女性中,综合代谢异常的存在与眼部并发症、周围神经病变、慢性肾病和 CVD 的存在密切相关,并根据年龄、糖尿病病程和 HbA 1c进行校正。
结论/解释
1 型糖尿病患者越来越多地发现超重、肥胖和综合代谢异常,进一步增加了微血管和大血管并发症的风险。早期识别合并代谢异常的存在应使治疗干预措施能够向多因素方法进行调整,除了严格血糖控制和强化抗高血压药物和他汀类药物的使用外,还应注意避免超重的教育(例如饮食咨询)。应更彻底地探索在该人群中使用辅助疗法作为工具,以降低并发症的风险。


















































 京公网安备 11010802027423号
京公网安备 11010802027423号